Scroll to:
Minimally invasive surgical treatment of female hypospadias and urethral hypermobility complicated by postcoital dysuria
https://doi.org/10.21886/2308-6424-2021-9-1-72-79
Abstract
Introduction. Currently, a large number of different surgical methods have been developed for the treatment of postcoital dysuria caused by hypospadias and urethral hypermobility. However, the literature does not reflect clear criteria and indications for a particular treatment method. Various modifications of the traditional urethral transposition can be accompanied by traumatic injury to the abundantly innervated paraclittoral and paraurethral zones, which provokes sexual disorders, up to anorgasmia. The search continues for new, effective, but less invasive techniques compared to traditional surgical transposition.
Purpose of the study. To assess the efficacy and safety of a combined technique: removal of urethra-hymenal adhesions along with a paraurethral injection of gel filler.
Materials and methods. 83 patients with hypospadias and urethral hypermobility complicated by postcoital dysuria were treated since 2015. The age ranged from 17 to 40 years. Examination revealed urethro-hymenal adhesions of varying severity and positive O’Donnell-Hirschhorn test in all women. One patient had previously undergone urethral transposition with a temporary effect. All women underwent surgical treatment, which consisted of the urethro-hymenal adhesions removal and suburethral injection of hyaluronic acid-based filler. The bulking gel (1-2 ml) was injected in a fan-shaped manner paraurethrally in from the point at 6 o'clock of the conventional dial. Thus, a «gel pad» was created, which lifts the meatus and the distal urethra, limiting their mobility and traumatization during intercourse. No complications were observed. The postoperative examination was performed after 1, 6, 12 months.
Results. An improvement in the quality of life was noted in 74 patients (89%) (UDI 6 and PISQ-12 questionnaires). The external urethral orifice was not displaced inwards, the urethra projected above the vaginal entrance during the vaginal examination and the O’Donnell-Hirschhorn test. In 13 (15.5%) patients, the biodegradation of the gel was accompanied by the return of symptoms of various degrees in different terms after the operation (from 8 to 13 months). 8 women required repeat injections of the filler; four patients needed 2 injections and 1 patient needed three injections. The repeated manipulations were performed under local anaesthesia. In 8 cases (9.6%), continued urination disorders were noted despite the termination of the dominance of postcoital dysuria, which required additional complex treatment. Improvement of sexual life was observed in 89% of all operated women according to the described technique. Urethral transposition was not required in any of the patients.
Conclusions. The combined technique improves the treatment's results of female hypospadias and urethral hypermobility complicated by postcoital dysuria with minimal development risk of complications. The disadvantage is the natural bulking gel biodegradation, which may necessitate its reimplantation.
Keywords
For citations:
Snurnitsyna O.V., Inoyatov Zh.Sh., Lobanov M.V., Malinina O.Yu., Rapoport L.M., Enikeev M.E. Minimally invasive surgical treatment of female hypospadias and urethral hypermobility complicated by postcoital dysuria. Urology Herald. 2021;9(1):72-79. (In Russ.) https://doi.org/10.21886/2308-6424-2021-9-1-72-79
Introduction
The problem of recurrent infection of the lower urinary tract remains one of the most acute issues in urology [1]. 1 out of 3 women by the age of 24 had a minimum of one episode of acute cystitis according to statistical data, and in half of them, this process becomes recurrent [1][2][3]. Postcoital cystitis is observed in 60% of cases of recurrent infections of the lower urinary tract [4].
Female hypospadias and urethral hypermobility, presence of urethral-hymenal adhesions, and a degree of sexual activity are some of the most frequent causes of postcoital dysuria [5][6][7]. Urethral-hymenal adhesions are congenital adhesions or fusions between the residuals of the hymen of different shapes and sizes and the walls of the external urethral orifice [8].
Postcoital dysuria is a psychological problem often rather than medical [9][10]. Low efficacy of conservative therapy and long-term course of the disease lead to emotional and psychic disorders. Some patients who have a recurrence and dyspareunia after each sexual intercourse have to refuse sexual life. There are different modifications of surgical treatment for female hypospadias. The methods aim to limit the mobility of the urethra during intercourse, maximally transposition the urethral orifice from the vaginal opening to the clitoris [10]. Low traumatic isolated removal of urethral-hymenal adhesions is low effective [11][12]. Traditional urethral transposition has such significant disadvantages as traumatization of the vaginal opening, paraurethral, and paraclitoral tissues during the mobilization and distal urethral transposition [13][14]. The invasiveness of these surgeries can result in the appearance of cicatricle changes in the vaginal opening, dyspareunia, and anorgasmia [14][15]. It is necessary to search for new low invasive and less traumatic methods that are as effective as urethral transposition. The study aimed to evaluate the effectiveness and safety of the combined minimally invasive method of treatment for female hypospadias and urethral hypermobility ― removal of urethral-hymenal adhesions and paraurethral implantation of a filler.
Materials and methods
83 patients aged 17 ‒ 40 years old with female hypospadias and urethral hypermobility complicated by postcoital dysuria have been treated since 2015. The disease onset was registered with the beginning of sexual life in 60 (80%) women out of 83, with the beginning of regular sexual life ― in 15 (20%) women. The examination showed that all women had urethral-hymenal adhesions, positive O᾽Donnell-Hirschhorn test, and vaginal dystopia of the urethra. One patient had a previous urethral transposition that had a temporary effect. All women underwent surgical treatment. They had urethral-hymenal adhesions dissected and received a suburethral injection of hyaluronic acid filler according to the patented method (patent for invention No. 2660993 dated July 11, 2018).
The method consists of 2 stages. The first stage includes a dissection of urethral-hymenal adhesions. For this, the residuals of the hymen and urethral-hymenal adhesions were removed (Fig. 1A, 1B). The wound was sutured with two continuous absorbable sutures Vicryl 5 – 6/0 (Fig. 2).

Figure 1. Removal of hymenal residuals and urethral-hymenal adhesions along the hymen lower surface (A), paraurethral (B)

Figure 2. Wound suturing
The second stage included urethral transposition through suburethral injection of the filler. Recombinant biodegradable hyaluronic acid was injected in a fan-like manner (1 ‒ 3 ml) from the point at five, six, seven-eight hours o’clock of the conventional clock dial (Fig. 3).

Figure 3. Suburethral filler injection: A – at the point on the five o’clock conditional clock-dial; B – at the point on the six o’clock conditional clock-dial; C – at the point on the seven-eight o’clock conditional clock-dial.
The authors used high-density biphase hyaluronic acid filler for injections based on cross-linked hyaluronic acid of non-animal origin with intramolecular links.
There are presently no profile questionnaires for postcoital dysuria caused by the hypermobility of the urethra and hypospadias, so the quality of life was evaluated using a questionnaire UDI-6 (urogenital distress inventory ― 6) and PISQ-12 (pelvic organ prolapse/urinary incontinence sexual questionnaire ― 12). Question 8 about urogenital prolapse was excluded from the questionnaire PISQ-12. Questions 3 and 5 about stress urine incontinence were excluded from the questionnaire UDI-6. The survey was performed before surgery and 1, 6, and 12 months after surgery. It was supplemented with laboratory tests, vaginal examination, and the O᾽Donnell-Hirschhorn test.
The statistical analysis of the data was performed using the software package IBM SPSS Statistics 22.0. To reveal associations between numerical characteristics and the results of the treatment, Spearman’s rank correlation was used. Confidential intervals were calculated based on the binomial distribution. The differences were considered significant (statistically significant) at p = 0.05.
Results
The disease onset was registered with the beginning of regular sexual life in 50 patients. Cystitis manifested right after the first sexual intercourse in 32 patients.
The quality of life, evaluated through a survey (questionnaires UDI-6 + PISQ-12 (Sexual Questionnaire), improved in 74 patients (89%) (p < 0.05) (Fig. 4, 5).
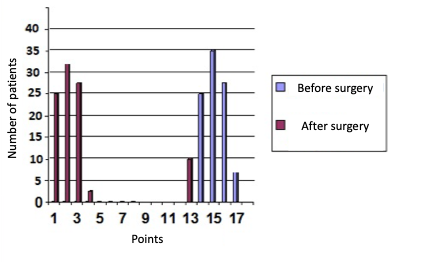
Figure 4. Distribution of patients according to UDI-6 points before and after surgery (p < 0.05)
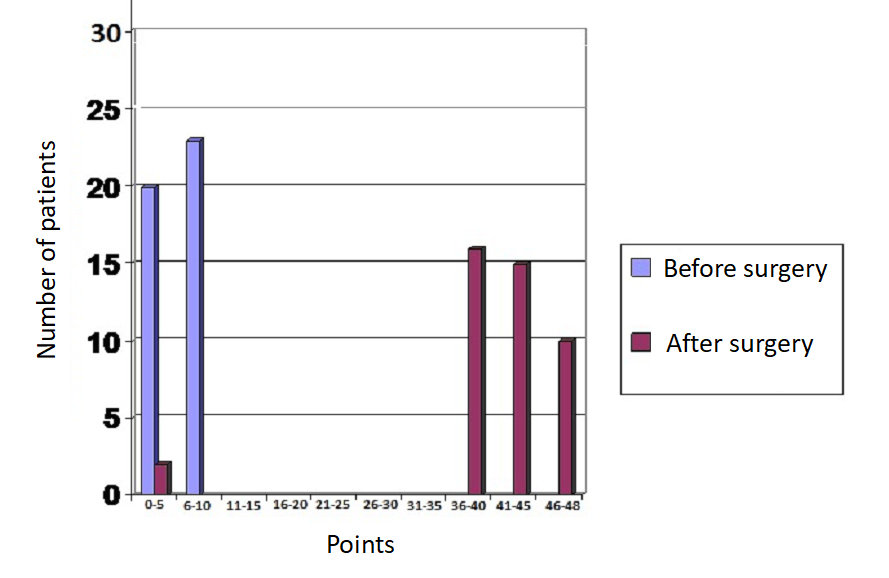
Figure 5. Distribution of patients by PISQ-12 points before and after surgery (p < 0.05)
Vaginal examination showed that during Hirschhorn’s test, the outer urethral orifice did not move inside. The urethra was projected above the vaginal opening. A gel pad, which prevented the hypermobility of the urethra during sexual intercourse, was visualized under the urethra (Fig. 6).

Figure 6. Postoperative view: the gel pad formed after the filler injection is visualized under the urethra
The injected gel biodegraded in 13 patients in different periods after the surgery (8 ‒ 13 months), which required repeated injection of the filler under local anesthesia. The injection of the filler did not have the desired effect in one patient who underwent the previous transposition of the urethra.
Despite the resolution of postcoital dysuria, other urination disturbances required additional complex treatment in eight cases (9.6%). The improvement of sexual life was observed in 89% of women who were operated on by the described method. The urethral transposition was not required in any of these cases. Intra and postoperative complications (including dyspareunia) were not observed.
Discussion
Hirschhorn described urethral-hymenal adhesions (residuals of the hymen) as the cause of postcoital cystitis in 1965 [10]. The urethra involved in the sclerotic process forms a common adhesion with the residuals of the hymen. Significant hymenal adhesions are closely connected with the distal urethra. They contribute to the urethral invagination during intercourse due to their sizes and lead to painful sexual intercourse, which reduces the quality of life of patients. Transposition of the urethral outer orifice into the vagina occurs during frictions. This leads to a retrograde penetration of the vaginal microflora into the urethra, which is a constant source of infection of the lower urinary tract [10]. Besides, excessive (hypertrophied) residuals of the hymen tightly close the vaginal opening, which can provoke the development of chronic vulvovaginitis because of the lack of oxygen [11]. Taking into account a common lymphatic collector, such conditions aggravate the risks of persisting inflammation of the lower urinary duct. As a result, persistent chronic “postcoital cystitis” develops [12].
O’Donnel, who connected the disease with ectopia of the urethra, proposed a surgical technique on the urethral outer orifice transposition in the case of its ectopia from the vagina to the paraclitoral area in 1968. The method was called a urethral transposition [13].
Several modifications of the urethral transposition have been developed. The main techniques include extravaginal urethral transposition [6], distal urethral transposition [14], and urethral meatus transposition [15][16]. The proposed methods are based on the outer urethral orifice transposition from the vaginal opening towards the clitoris. However, these techniques are associated with excessive tissue traumatization, which can lead to the formation of cicatrices in the vaginal opening, innervation impairment, tunnel syndromes, strictures, tension, and urethral detachment [17]. According to other authors, surgical intervention in the paraclitoral area is also associated with the development of chronic pelvic pain syndrome, dyspareunia, and anorgasmia [18][19].
Complications after reconstructive and esthetic surgeries on the vaginal opening and paraclitoral areas in adults and adolescents raise concern in the American Association of Obstetricians and Gynecologists [20]. There are presently not enough studies on long-term results that show the satisfaction of patients in the postoperative period, safety, and rate of complications [20].
Ampt (2013) performed a 10-year analysis of complications after surgeries on the vaginal opening. The rate of complications was 7.2%. The most frequent complications included non-specific inflammatory changes of the lower urinary tract, dyspareunia, and long-term pain syndrome in the area of postoperative wounds. Each 23rd observation required repeated surgical intervention because of poor wound regeneration or unsatisfactory treatment results [21].
The proposed method included 2 components: dissection of urethral-hymenal adhesions and restoration of normal anatomy of the urethra through the injection of the filler (bulk gel). Atraumatic distal urethral meatus transposition is provided by the formation of a gel pad. The mobility of the distal urethra decreases and the distance from the vaginal opening to the urethra orifice increases. The separation of the meatus and the vaginal opening by dissection of urethral-hymenal adhesions and residuals of the hymen and the injection of the filler leads to a significant decrease in the degree of urethral invagination during coitus.
Additional therapeutic mechanism during the formation of a gel pad includes a stop (limitation) of lymphogenic exchange between the vagina and the lower urinary tract, which decreases the risk and degree of postcoital inflammation of the urinary tract.
The results of the present study demonstrate the high effectiveness of the treatment for female hypospadias and hypermobility of the urethra complicated by postcoital dysuria. The recurrence was observed only after natural biodegradation of the filler. The questionnaires UDI-6 and PISQ-12 provided evidence of subjective improvement in the condition of patients after surgery.
The main drawback of the proposed method is the natural biodegradation of the bulk gel, which may require repeated injection. It was observed in eight patients in the present study (12.7%). Still, the repeated manipulation can be made under local anesthesia in outpatient conditions. The method is characterized by the lack of intra- and postoperative complications. The worsening of the quality of life and sexual function was not registered.
Conclusion
The proprietary method improves the results of the treatment of patients with hypospadias and hypermobility of the urethra, complicated by postcoital dysuria, with a minimum risk of complications. Taking into account the lack of complications and minimally invasive character, the dissection of the urethral-hymenal adhesion and injection of the filler can become the method of first-line in women with postcoital cystitis. The method is not associated with significant tissue fibrosis, and as a result, does not increase the technical complexity and risks of traditional urethral transposition if it is required in the future. The drawback of the method is the natural biodegradation of the filler (bulk gel), which may require its re-implantation.
References
1. Dason S, Dason JT, Kapoor A. Guidelines for the diagnosis and management of recurrent urinary tract infection in women. Can Urol Assoc J. 2011;5(5):316-22. DOI: 10.5489/cuaj.11214
2. Bergamin PA, Kiosoglous AJ. Non-surgical management of recurrent urinary tract infections in women. Transl Androl Urol. 2017;6(Suppl 2):S142-S152. DOI: 10.21037/tau.2017.06.09
3. Loran O.B. Zajcev A.V., Godunov B.N., Kaprin A.D., David'yanc A.A. Sovremennye aspekty diagnostiki i lecheniya hronicheskogo cistita u zhenshchin. Urologiya i nefrologiya. 1997;6:7-14. (In Russ.). eLIBRARY ID: 24135237
4. Stamatiou C, Bovis C, Panagopoulos P, Petrakos G, Econo-mou A, Lycoudt A. Sex-induced cystitis--patient burden and other epidemiological features. Clin Exp Obstet Gynecol. 2005;32(3):180-2. PMID: 16433159
5. Derevyanko I.M. Ryzhkov T.I., Eliseeva V.V. Vlagalishchnaya ektopiya uretry i mochepolovoj sinus u zhenshchin. Stavropol'; 2004. (In Russ.).
6. Komyakov B.K. Rezul'taty 228 ekstravaginal'nyh transpozicij uretry. Urologicheskie vedomosti. 2017;7(S):54-55. (In Russ.). eLIBRARY ID: 29246473
7. Schaeffer AJ, Stamey TA. Studies of introital colonization in women with recurrent urinary infections. IX. The role of antimicrobial therapy. J Urol. 1977;118(1 Pt 2):221-4. DOI: 10.1016/s0022-5347(17)57950-1
8. Hirschhorn RC. Urethral-hymenal fusion. J Urol. 1966;96(5):784-9. DOI: 10.1016/s0022-5347(17)63350-0
9. Krupin V.N. Belova A.N. Hronicheskaya tazovayabo' Moskva; 2007. (In Russ.).
10. Permyakov A.N. Uretral'nyj sindrom u zhenshchin. Avtoref. diss. kand. med. nauk. Moskva; 1983. (In Russ.).
11. Reed JF Jr. Urethral-hymenal fusion: a cause of chronic adult female cystitis. J Urol. 1970;103(4):441-6. DOI: 10.1016/s0022-5347(17)61977-3
12. Barr SJ. Urethral-hymenal fusion: a cause of postcoital cystitis. Am J Obstet Gynecol. 1969;104(4):595-7. DOI: 10.1016/s0002-9378(16)34254-5
13. O'DONNELL RP. Relative hypospadias potentiated by inadequate rupture of the hymen: a cause of chronic inflammation of the lower part of the female urinary tract. J Int Coll Surg. 1959;32:374-88. PMID: 14428066
14. Gumin L.M., D'yakov V.V., Gvozdev M.YU. Transpoziciya distal'nogo otdela uretry v operativnom lechenii recidiviruy-ushchih infekcij nizhnih mochevyh putej. Rossijskij vestnik akushera-ginekologa. 2008;8:S9:15. (In Russ.). eLIBRARY ID: 11520847
15. Stoiko Yu.M., Nesterov S.N., Kisamedenov N.G., Rogachikov V.V., Ilchenko D.N., Brook Yu.F. Surgical treatment of recurrent infections of lower urinary tract in females. Vestnik Nacional'nogo mediko-hirurgicheskogo centra im. N.I. Pirogova. 2009;4(2):53-56. (In Russ.). eLIBRARY ID: 12970767
16. Ronzoni G, De Giovanni L, Weir JM, Pasqui F, Menchinelli P. Transposing the urethral meatus in the treatment of recurrent and postcoital cystitis in women with hypospadias. BJU Int. 2001;87(9):894-6. DOI: 10.1046/j.1464-410x.2001.01903.x
17. Gyftopoulos K, Matkaris M, Vourda A, Sakellaropoulos G. Clinical implications of the anatomical position of the urethra meatus in women with recurrent post-coital cystitis: a case-control study. Int Urogynecol J. 2019;30(8):1351-1357. DOI: 10.1007/s00192-018-3710-7
18. Goodman MP, Placik OJ, Benson RH 3rd, Miklos JR, Moore RD, Jason RA, Matlock DL, Simopoulos AF, Stern BH, Stanton RA, Kolb SE, Gonzalez F. A large multicenter outcome study of female genital plastic surgery. J Sex Med. 2010;7(4 Pt 1):1565-77. DOI: 10.1111/j.1743-6109.2009.01573.x
19. Wilkie G, Bartz D. Vaginal Rejuvenation: A Review of Female Genital Cosmetic Surgery. Obstet Gynecol Surv. 2018;73(5):287-292. DOI: 10.1097/OGX.0000000000000559
20. Committee on Gynecologic Practice, American College of Obstetricians and Gynecologists. ACOG Committee Opinion No. 378: Vaginal "rejuvenation" and cosmetic vaginal procedures. Obstet Gynecol. 2007;110(3):737-8. DOI: 10.1097/01.AOG.0000263927.82639.9b
21. Ampt AJ, Roach V, Roberts CL. Vulvoplasty in New South Wales, 2001-2013: a population-based record linkage study. Med J Aust. 2016;205(8):365-369. DOI: 10.5694/mja16.00512
About the Authors
O. V. SnurnitsynaRussian Federation
Olesya V. Snurnitsyna — M.D., Urologist; Institute for Urology and Reproductive Health.
119991, Moscow, 2 Bolshaya Pirogovskaya st.; tel. +7 (916) 425-16-43
Competing Interests:
no conflicts of interest
Zh. Sh. Inoyatov
Russian Federation
Zhasur Sh. Inoyatov — M.D., Urologist; Institute for Urology and Reproductive Health.
119991, Moscow, 2 Bolshaya Pirogovskaya st.
Competing Interests:
no conflicts of interest
M. V. Lobanov
Russian Federation
Mikhail V Lobanov — M.D., Urologist; Institute for Urology and Reproductive Health.
119991, Moscow, 2 Bolshaya Pirogovskaya st.
Competing Interests:
no conflicts of interest
O. Yu. Malinina
Russian Federation
Olga Yu. Malinina — M.D., Cand.Sc. (M); Urologist.
111020, Moscow, 2 Gospital'naya sq.
Competing Interests:
no conflicts of interest
L. M. Rapoport
Russian Federation
Leonid M. Rapoport — M.D., Dr.Sc.(M), Full Prof; Urologist, Institute for Urology and Reproductive Health.
119991, Moscow, 2 Bolshaya Pirogovskaya st.
Competing Interests:
no conflicts of interest
M. E. Enikeev
Russian Federation
Mikhail E. Enikeev — M.D., Dr.Sc.(M), Full Prof; Urologist, Institute for Urology and Reproductive Health.
119991, Moscow, 2 Bolshaya Pirogovskaya st.
Competing Interests:
no conflicts of interest
Review
For citations:
Snurnitsyna O.V., Inoyatov Zh.Sh., Lobanov M.V., Malinina O.Yu., Rapoport L.M., Enikeev M.E. Minimally invasive surgical treatment of female hypospadias and urethral hypermobility complicated by postcoital dysuria. Urology Herald. 2021;9(1):72-79. (In Russ.) https://doi.org/10.21886/2308-6424-2021-9-1-72-79













































