Scroll to:
Ejaculation-sparing enucleation of benign prostate hyperplasia: is it almost feasible?
https://doi.org/10.21886/2308-6424-2023-11-1-59-69
Abstract
Introduction. Patients often request maintenance of antegrade ejaculation, and try to find the clinic, surgeon, and treatment to store it. Despite an established technique, the long-term results of ejaculation-sparing operations at a large prostate volume remain unstable. This is not allowed to give patients a guarantee in maintaining this component in their sexual life.
Objective. To evaluate the frequency of ejaculation maintenance after laser ejaculatory-sparing prostate enucleation.
Materials & methods. Since 2017 ejaculation-sparing laser enucleations have been performed in prostate volume (V pr > 80 cc) in 84 patients. Fifty-four patients (64%) had three lobes benign prostate hyperplasia (BPH) and two lobes — 30 patients (36%). Preoperative voiding parameters were IPSS score — 21.0 ± 2.7, QoL — 4.8 ± 0.6, residual urine volume (V res) — 139 ± 43 mL, Q max — 8.1 ± 2.0 mL. We estimate the result as positive if antegrade ejaculation remained after intervention. If ejaculation volume decreased, then as partially positive and negative — ejaculation was absent postoperatively. We conducted questionnaire and follow-up examination 3 – 6 months after intervention.
Results. Thulium-fiber laser enucleations have been performed in all cases without any serious complications. Followup 3 – 6 months after operation showed V pr — 29 ± 4 cc, V res — 19 ± 17 mL, Q max — 19.1 ± 3.1 mL/sec. IPSS score — 8.1 ± 1.9 and QoL — 2.6 ± 0.7. There are the following technical remarks: 1) tissue-sparing in the verumontanum; 2) no or minor mechanical tissue tension during enucleation; 3) avoid additional resection in the bladder neck; 4) refuse total coagulation; 5) no urethral catheter tension after operation; 6) catheter balloon inflow only in the bladder, not in the fossa. Antegrade ejaculation has stored at 17 (20%) patients, partial ejaculation — at 34 (40%) patients, so overall efficacy is 60%. The presence of a median lobe is shown to be negative prognostic factor due to the absence of full antegrade ejaculation in all cases. A partial ejaculation was achieved at 21 patients. Based on the obtained results we have optimized the three-lobe prostate enucleation technique. Four from our initial 7 patients had full storage of ejaculation and 3 — partial.
Conclusion. The possibility of BPH laser surgery to store ejaculation function at the request of the patients is modest. The presence of the median lobe makes the full ejaculation-sparing impossible. In cases of two lobes BPH full storage of the ejaculation was at 57% and partial at 43%, respectively. The following evaluation of the described technique is mandatory.
Keywords
For citations:
Martov A.G., Ergakov D.V., Asliev K.A., Baykov N.A. Ejaculation-sparing enucleation of benign prostate hyperplasia: is it almost feasible? Urology Herald. 2023;11(1):59-69. (In Russ.) https://doi.org/10.21886/2308-6424-2023-11-1-59-69
Introduction
The persistent deterioration of sexual life because of surgical treatment of benign prostatic hyperplasia (BPH) due to the development of retrograde ejaculation is a typical consequence. Urologists are aware of it, and patients are informed before surgical interventions [1–11].
According to the academic literature, the frequency of retrograde ejaculation after transurethral resection reaches 80 – 100% [1]. For a long time, the onset of retrograde ejaculation after surgery was explained by the resection of tissues in the neck of the bladder and the destruction of the internal bladder sphincter. Alloussi showed that for the preservation of natural ejaculation, the preservation of tissues around the seminal tubercle was more important than resection of tissues in the neck [2]. As criteria for the possibility of predicting the preservation of ejaculatory function, the author of the method indicates the prostate volume up to 50 cc and the absence of an average lobe.
The introduction of electrosurgical and laser enucleation into clinical practise has led to a gradual decrease in the use of transurethral resection of the prostate, which is associated with a lower incidence of hemorrhagic complications and postoperative relapses after enucleation [1][3][4].
Despite awareness of the high probability of ejaculation disorders, a large cohort of patients is interested in their preservation. Therefore, for each of the methods of removal of adenomatous tissues (incision, vaporization, resection, and enucleation), the active development of ejaculatory-sparing techniques, for example, ejaculatory-sparing vaporization, continues, as well as the active search and introduction into practice of new minimally invasive methods (Urolift®, water jet ablation) [3][4].
It is important to consider that the chances of maintaining antegrade ejaculation during ejaculatory-protective enucleation are lower than the desired indicators, as in most cases there is an average proportion and the prostate volume is greater than 50 cc. This is the basis for research as the new options for the performing technique of this surgery is urgent.
The study aimed to evaluate the frequency of preservation of antegrade ejaculation after laser prostate enucleation performed in the ejaculatory-sparing variant and further optimisation of the procedure to perform surgery according to the data obtained.
Materials and methods
Since 2017, 84 patients with BPH have undergone transurethral thulium laser enucleation of the prostate gland in the standard for transurethral resection ejaculatory-protective variant with intact hyperplastic tissue 1 – 1.5 cm around the seminal tubercle [2][10] since the Pletnev City Clinical Hospital — Moscow Healthсare Department [2][10]. After the surgical intervention was completed, the bladder was drained with a three-way urethral catheter, while the balloon of the urethral catheter was inflated in the bladder cavity. The tension of the urethral catheter was not performed. With a smooth course of the postoperative period, the flushing system was turned off on the first day and the removal of the urethral catheter was performed the second day after surgery.
The indications for the inclusion of patients in the study were the following: preserved erectile function before surgery (assessed according to the international erectile function questionnaire ICEF-5 with the addition of questions 9 and 10 from ICEF-15) and the desire to preserve natural ejaculation. The age of patients was from 48 to 72 years (cf. 59 ± 6 years). The volume of the prostate gland was 96 ± 8 (82 – 113) cm3.
All the patients underwent a standard comprehensive clinical and laboratory medical examination. The prostate-specific antigen (PSA) index before surgery was 5.26 ± 2.32 ng/ml (1.2 – 6.5 ng/ml). According to the PSA indicators, 64 (76%) patients underwent prostate biopsy, as a result, the diagnosis of prostate hyperplasia was morphologically verified.
To make a correct comparison, all the surgeries were performed using a thulium fibre laser FiberLase U3 (IPG Photonics Corp., IRE-Polus, Fryazino, Russia) in the mode of 4 J, 15 Hz (60 W), with a laser fibre of 550 microns.
All the patients underwent transurethral surgery by two urologists with extensive experience in performing endourological interventions, including ejaculatory-protective transurethral resection and prostate enucleation. The accumulated experience of such surgeries made it possible to divide patients depending on the presence of an average fraction. In the large-glands group, 30 patients (36%) did not have an average proportion, the remaining 54 patients (64%) had a three-lobed form of hyperplasia nodule growth, that is, 64% of patients had both negative signs, based on which they were informed during consultation about the high probability of no effect of ejaculatory-protective surgery.
The results of treatment were evaluated 3 to 6 months after the surgeries, special attention was paid to the cancellation of postoperative medicine therapy, a1-blockers particularly. The surgical effectiveness was positive in the cases with complete preservation of natural ejaculation; partial — with a decrease in the ejaculate volume and the detection of spermatozoa in urine analysis after the act of ejaculation, and negative — in the absence of antegrade sperm ejaculation.
Statistical analysis. Data processing was carried out using the program Statistica ver. 13.0 (StatSoft Inc., Tulsa, OK, USA). Therefore, Figure 1 shows the general scheme of the study. Initially, before each statistical analysis, the normality of the distribution of the results obtained in the variation series of each group was determined using the Kolmogorov-Smirnov criterion. While statistically comparing the quantitative parameters of two analyzed aggregates, unrelated samples obeying the law of normal distribution, the Fisher t-test (p) was used. When comparing two dependent (paired) parameter samples, the Fisher paired t-test was used. The critical level of reliable significance of the analyzed statistical hypotheses in the study was taken to be less than 0.05 (p< 0.05).
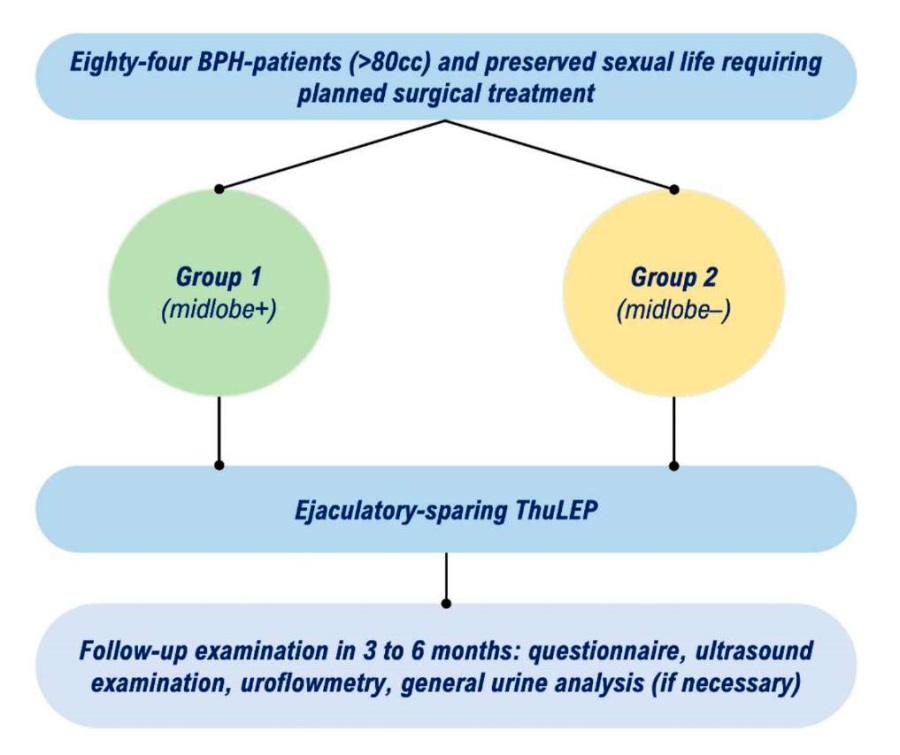
Figure 1. General study design (flow-chart) to assess the preservation of antegrade ejaculation after BPH laser enucleation
Results
Table 1 shows the results of the treatment of patients of both groups 3 to 6 months after surgery. The assessment of changes in standard subjective and objective indicators of pre- and postoperative parameters is given in Table 2, because of which it can be concluded about the high quality of urination and life of patients included in the study.
Table 1. Frequency of antegrade ejaculation maintenance after ejaculation-sparing laser enucleation
|
Outcome |
Group 1 (n = 54) |
Group 2 (n = 30) |
|
Fully saved, n (%) |
0 |
17 (57) |
|
Relatively saved, n (%) |
21 (39) |
13 (43) |
|
Absent, n (%) |
33 (61) |
0 |
Table 2. Subjective and objective voiding parameters before and 3–6 months after ejaculation-sparing enucleation
|
Period |
Indicators |
|||
|
V pr cm3 |
IPSS – QoL scores |
Q max mL/sec |
V res mL |
|
|
Before surgery |
96 ± 8 |
21 ± 2.7 – 4.8 ± 0.6 |
8,1 ± 2,0 |
139 ± 43 |
|
After surgery |
29 ± 4* |
8.1 ± 1.9 – 2.6 ± 0.7* |
19.1 ± 3.1* |
19 ± 17* |
Notes:
- IPSS – International Prostate Symptoms Score; Q max – maximum urinary flow rate; V pr – prostate volume; V res – residual urine volume
- *p < 0.05 (estimated using Fisher's exact test)
In the group with the presence of the average lobe, which prevailed in the present observation, no (!) case demonstrated complete antegrade ejaculation. A partial positive result was observed in 39% of cases and 61% of patients had retrograde ejaculation.
In the second group, which consisted of 30 patients, antegrade ejaculation was observed in 57% of patients and partial ejaculation in 43% of patients.
The authors of this study believe that the removal of the middle lobe is key to the preservation of antegrade ejaculation. Therefore, because of our work, the technique of the operation was changed in such a way as to avoid the complete removal of the middle lobe. The essence of the proposed changes is not to remove the sub-bladder part of the middle lobe, but to remove only the intravesical part of it. The authors of this study performed a similar surgery with a thulium fibre laser in 7 patients (from 63 to 79 years old) with a prostate volume above 80 cc, who were not included in this study. In 4 – 6 months after the operation, 4 of them had completely preserved their natural ejaculation, and 3 had partial ejaculation. Considering this, it is necessary to dwell in more detail on the modified technique of surgery.
The first stage of the surgery was urethrocystoscopy, which allowed assessing the condition of the urethra and bladder. When a narrow urethra was detected, the preventing atraumatic use of the laser resectoscope 26 F, urethrotomy was performed according to Otis. While examining the bladder and detecting stones or neoplasms, they were crushed or removed in a single block.
Secondly, the surgical area and hyperplastic lobes were examined, the degree of their intravesical growth was assessed, and the boundaries along which it was most convenient to separate the lobes from each other were determined. The shape of the apical zone, the distance from the external sphincter, the zone of the anterior commissure, and the boundaries between the lobes were also determined. Special attention was paid to the examination of the zone of the seminal tubercle; if possible, the surgeons tried to visualize the places of the opening of the ejaculatory ducts (Fig. 2). This zone should remain intact and undamaged during mechanical traction of tissues, under the energetic influence of the laser, and during the final hemostasis. Considering that for the preservation of sexual life, the issue of urine retention is also important, during ejaculatory-protective surgery, a large role was assigned to the preservation of the external sphincter. Therefore, the surgery was started at 12h in the area of anterior commissure. Next, an incision of the mucosa was made in the shape of a horseshoe with extension to the expected level of the capsule and expansion of 2h to 10h of the conventional dial (Fig. 3A). The reference point for the dissection was the level of the seminal tubercle, after which the instrument was turned over for 12h and the dissection of the prostatic urethra mucous membrane was performed directly at this level.
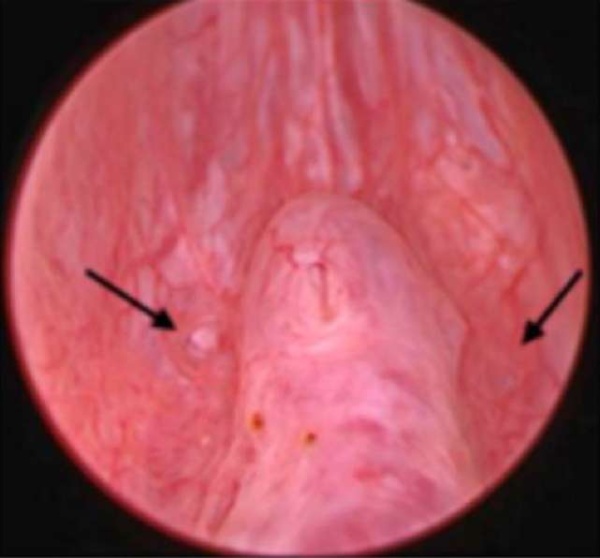
Figure 2. Endoscopic view: verumontanum and orifices of ejaculatory ducts (arrows)
The next stage of the surgery was the incision of the mucosa on the right side (or on the left one, as it was convenient) of the seminal tubercle; it was important to avoid crossing the sperm ejection zones. To do this, the mucosa and the underlying hyperplastic tissue were dissected at least 1.5 cm laterally to the right and left of the seminal tubercle. The prostatic urethra mucous membrane was dissected (Fig. 3B), and therefore the middle lobe was separated from the left lobe. To do this, it was necessary to reach the capsule level with the help of laser energy and a minimum of mechanical effort. Then, following in a counterclockwise direction, the mucosa and hyperplastic tissue were dissected in the apex area of the left lobe to combine the incisions along the circumference. Thus, the apical part of the left lobe was completely separated from the external sphincter (Fig. 3C). After the apex was isolated, it was possible to separate the mucosal zone in the neck area, which was best achieved by moving in the direction of the dial arrow (Fig. 3D), the latter was possible and antegraded from the apex to the bladder neck.
The final stage was the unification of the discharge planes at the apex and bladder, leading to displacement of the left lobe into the lumen of the bladder (Fig. 3E). It is important to note that to preserve antegrade ejaculation, no additional dissection of the bladder neck is performed (Fig. 3F).
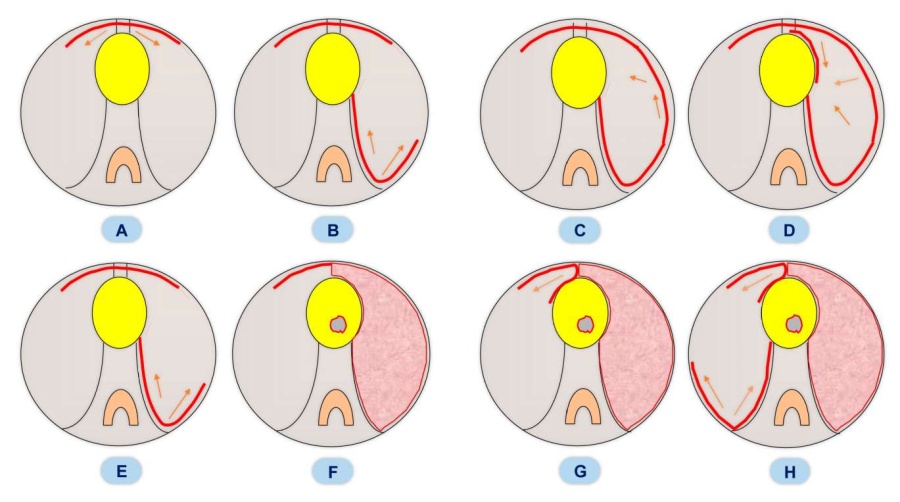
Figure 3. Stages of ejaculatory-sparing enucleation (part 1): A – horseshoe-shaped incision of the mucosa in the anterior commissure area at the level of the seminal tubercle; B – left lobe preparation from the middle lobe; C – apex zone separation in the left lobe area; D – left lobe separation from the bladder neck; E – left lobe enucleation into the bladder cavity; F – bladder neck sparing; G – right lobe preparation by the top-down method; H – right lobe separation the from the middle one
After the removal of the left lobe, intermediate hemostasis was performed using laser energy to maintain good endoscopic visibility to avoid perforation of the capsule, the bladder neck area, or damage to the external sphincter.
The removal of the right lobe can be started in the direction from 12h to 9h of the conventional dial (Fig. 3G), that is, from top to bottom, as well as in the usual way, as in the case of the left lobe (Fig. 3H). The 'top-down' method involves creating a single plane for enucleation from the bladder neck to the apex level, followed by connection to the mucosal dissection zone in the apex area, thus the lobe becomes more malleable and can be separated from the capsule even with minor mechanical movements of the instrument.
As in the case of the left lobe separation from the middle lobe at the stage of enucleation of the right lobe, it is advisable to avoid mechanical movements with the tool to avoid mechanical separation of the adenomatous tissues of the sub-bladder part of the middle lobe from the capsule. Therefore, at this stage, tissue dissection is performed only with the help of laser energy. The further stages of separation of the right lobe correspond to similar ones during the enucleation of the left lobe (Fig. 4A, 4B).
After the completion of enucleation of the right lobe, intermediate hemostasis is performed, which is necessary for better orientation (Fig. 4C).
After achieving good visibility, the removal of the middle lobe was started. To avoid mechanical injury of the sub-bladder part of the middle lobe, which could lead to its detachment from the capsule, the use of laser energy alone is also justified at this stage (Fig. 4D). With the help of a laser, the intravesical part of the middle lobe is cut off from the bladder neck at a distance of 0.5 cm from the neck level (Fig. 4E), which allows one to avoid, on the one hand, damage to the area of the ureteral mouths, and on the other, displacement of the incision zone into the prostatic urethra and damage to the sub-bladder part of the middle lobe and the bladder neck the itself. At the stage of separation of the tissues of the middle lobe from the neck, additional dissection of the bladder neck is also impractical.
After the morcellation of the removed tissues, the final hemostasis was performed; the use of electricity is undesirable. The final view of the surgery zone is shown in Fig. 4F.
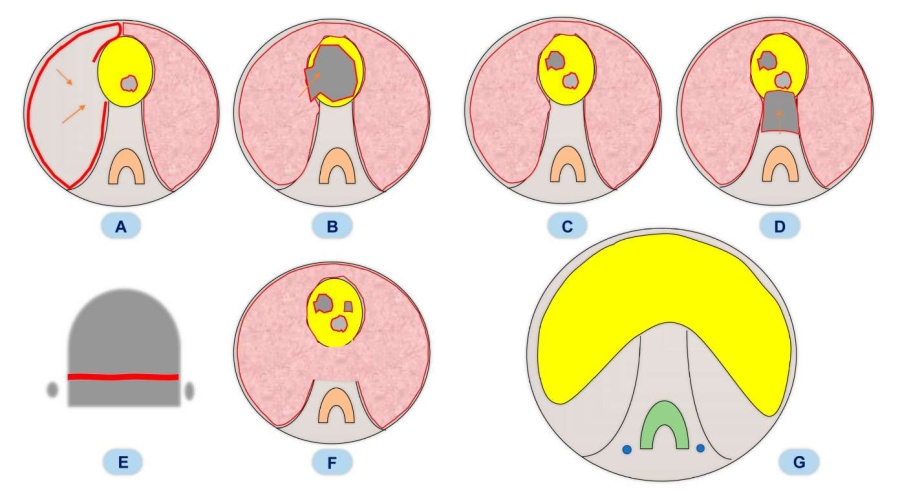
Figure 4. Stages of ejaculatory-sparing enucleation (part 2): A – joining of the enucleations level while moving from up- to downwards and down- to upwards and shifting tissues to the bladder neck; B – right lobe enucleation into the bladder cavity; C – intermediate hemostasis before the median lobe removal; D – median lobe removal; E – schematic view of the intravesical part of the median lobe removal; F – final schematic endoscopic view; G – schematic view of the ejaculation-sparing pyramid
Discussion
The study conducted by the authors of this article confirmed that the presence of an average lobe is the main prognostic factor for the development of retrograde ejaculation after surgery. This conclusion underlies the modification of the ejaculatory-sparing enucleation technique developed. Currently, the authors are conducting further studies aimed at studying its effect on the preservation of natural ejaculation in patients with a three-lobed form of hyperplasia nodule growth.
If the patient has a two-lobed form of growth, the use of even the standard technique of ejaculatory-protective enucleation with the leaving of an intact 1.5 cm zone around the seminal tubercle makes it possible to almost guarantee the complete safety of the ejaculatory function. At the same time, there are several factors that help to accelerate sexual rehabilitation of patients after protective and ejaculatory surgeries [3]. As the first factor, one should note the achievement of a significant improvement in subjective and objective indicators after surgery, that is, good control over postoperative symptoms of the lower urinary tract is desirable for the resumption of sexual activity after surgery [4]. Among other factors that matter in this case, testosterone levels, the state of erectile function before surgery, and the cancellation of alpha-blockers after surgery are important as well [5]. Only considering all the above-mentioned factors it is possible to increase the frequency of preservation of natural ejaculation after surgery. When age-related androgen deficiency or an initial decrease in erectile function is detected, the use of testosterone replacement therapy in combination with the use of type 5 phosphodiesterase inhibitors can increase the chances of resuming sexual activity and the safety of antegrade ejaculation [5]. No doubt, none of the above-mentioned factors can be a therapeutic way to treat retrograde ejaculation.
The indicator of fully or partially preserved ejaculation (61%) corresponds to published literature data. In a study by Herrmann and Wolters [6], the frequency of preserved ejaculation when using a solid-state thulium laser was 60%. In the another study by Kim et al., the degree of preservation of ejaculation was 49% [7]; the authors used a Ho:YAG laser. Therefore, Xu et al. reported reaching a retention rate of 76% [8], while noting differences in frequency depending on the structure of hyperplasia nodes. In the case of three lobes, the chances of maintaining natural ejaculation are lower than in the case of two lobes. Leonardi [9] also expressed the importance of separate isolation of patients with the presence of an average lobe, in which the effectiveness of a special technique of ejaculatory-protective laser vaporisation was evaluated.
The authors of the study have accumulated extensive experience in performing transurethral ejaculatory-sparing operations, the first results of which were published back in 2014 [10]. In this work, the authors used the same principles of ejaculatory-sparing resection of the prostate gland to perform enucleation, but the results showed that to achieve similar results when performing enucleation in a large-glands group, the preservation of the seminal tubercle zone alone was not enough.
The work of a group of authors led by. Popov [11] resulted in changes in ejaculatory function in patients after using various methods of treatment: transurethral resection, holmium, and bipolar enucleation, and endovideosurgical simple prostatectomy. One of the interesting conclusions of this work is the fact that ejaculatory disorders were present in 27–38% of patients before surgical treatment, which should certainly be considered in the integral evaluation of the method results. The authors traced the dynamics of ejaculatory dysfunction after 3 and 6 months. The results showed that the frequency of retrograde ejaculation did not change after the use of modern methods of treatment. Therefore, it is possible that the effectiveness of ejaculatory-protective operations is higher since little attention is paid to assessing the state of this function before surgery.
The developed concept of antegrade ejaculation preservation allows the patient to relieve infravesical obstruction and ensure adequate quality of life. To achieve this goal, it is necessary to ensure the safety of the so-called ejaculatory pyramid, that is, the area of tissue between the seminal tubercle and the neck of the bladder (Fig. 4G).
It is difficult to overestimate the need for extended tissue preservation, since in some cases, when the lateral lobes are cut off from the average, damage to the ejaculatory ducts along their length is possible. On the other hand, leaving a large number of residual tissues in patients with initially large hyperplasia nodes increases the risk of the persistence of infravesical obstruction, which requires appropriate experience in performing such operations and the use of appropriate tests during the operation (taking the instrument beyond the sphincter zone to assess the size of floating tissues) and after the operation (the so-called 'pi-pi' test – visual evaluation of the thickness of the irrigation fluid jet after removing the tool). There are no indications in the literature on the comparison of postoperative PSA reduction during traditional and ejaculatory-protective enucleation, as well as differences in the frequency of clinically significant (Slavien-Dindo ≥ 3) postoperative bleeding. Of undoubted interest is also the study of the long-term results of such operations in a group of patients with large glands. It is important to trace the frequency of repeated surgeries in connection with false relapses of the disease since the latest data is extremely necessary to consult patients before performing ejaculatory-sparing operations.
Conclusion
The study conducted is only the first in this direction; the authors plan to disseminate the data obtained during enucleation in a group of patients with small and medium-sized glands, as well as to conduct a comparative study on changes in ejaculatory function in patients with large glands who were operated on using a modified technique. Of course, the authors will evaluate the long-term results of ejaculatory-sparing operations. The need for such studies is due to the natural desire of patients to maintain a high-quality sex life in the postoperative period.
References
1. Martov A.G., Merinov D.S., Kornienko S.I., Gushchin B.L., Ergakov D.V., Mustafaev E.M., Borisenko E.A. Postoperative urological complications of transurethral electrosurgical interventions on the prostate for adenoma. Urologiia. 2006;(2):25-32. (Russian). PMID: 16708585
2. Alloussi SH, Lang C, Eichel R, Alloussi S. Ejaculationpreserving transurethral resection of prostate and bladder neck: short- and long-term results of a new innovative resection technique. J Endourol. 2014;28(1):84-9. DOI: 10.1089/end.2013.0093
3. Gild P, Dahlem R, Pompe RS, Soave A, Vetterlein MW, Ludwig TA, Maurer V, Marks P, Ahyai SA, Chun FK, Lenke L, Ernst T, Fisch M, Rink M, Meyer CP, Becker A. Retrograde ejaculation after holmium laser enucleation of the prostate (HoLEP)-Impact on sexual function and evaluation of patient bother using validated questionnaires. Andrology. 2020;8(6):1779-1786. DOI: 10.1111/andr.12887
4. Martov A.G., Ergakov D.V., Turin D.E., Andronov A.S. Bipolar and laser endoscopic enucleation for large benign prostatic hyperplasia. Urologiia. 2020;(1):59-63. (In Russian). DOI: 10.18565/urology.2020.1.59-63
5. Martov A.G., Ergakov D.V. Age-related androgen deficiency and benign prostatic hyperplasia: how to improve the rehabilitation of patients after transurethral surgery? Urologiia. 2016;(6):110-117. (In Russian). eLIBRARY ID: 28129929; EDN: VIAGXC
6. Herrmann TRW, Wolters M. Transurethral anatomical enucleation of the prostate with Tm:YAG support (ThuLEP): Evolution and variations of the technique. The inventors' perspective. Andrologia. 2020;52(8):e13587. DOI: 10.1111/and.13587
7. Kim M, Song SH, Ku JH, Kim HJ, Paick JS. Pilot study of the clinical efficacy of ejaculatory hood sparing technique for ejaculation preservation in Holmium laser enucleation of the prostate. Int J Impot Res. 2015;27(1):20-4. DOI: 10.1038/ijir.2014.22
8. Xu C, Xu Z, Lin C, Feng S, Sun M, Chen J, Zheng Y. Holmium Laser Enucleation of the Prostate: Modified Two-Lobe Technique versus Traditional Three-Lobe Technique-A Randomized Study. Biomed Res Int. 2019;2019:3875418. DOI: 10.1155/2019/3875418
9. Leonardi R. The LEST technique: Treatment of prostatic obstruction preserving antegrade ejaculation in patients with benign prostatic hyperplasia. Arch Ital Urol Androl. 2019;91(1):35-42. DOI: 10.4081/aiua.2019.1.35
10. Martov A.G., Andronov A.S, Dutov S.V, Baykov N.A. Ejaculatory-protective transurethral resection of the prostate. Urologiia. 2014;(4):69-75. (In Russian). eLIBRARY ID: 22370362; EDN: SVNUNJ
11. Popov S.V., Skryabin O.N., Orlov I.N., Grin' E.A., Topuzov T.M., Kyzlasov P.S., Malevich S.M., Sushina I.V., Vyazovcev P.V. Copulative function of patients after transurethral and endovideosurgical interventions due to benign prostate hyperplasia. Experimental and Clinical Urology. 2017;(4):42- 48. (In Russian). eLIBRARY ID: 32362469; EDN: YNJPHC
About the Authors
A. G. MartovRussian Federation
Alexey G. Martov — M.D., Dr.Sc. (Med), Full. Prof., Corr. Member of the RAS; Head, Dept. of Urology and Andrology;
Head, Urology Division (Minimally Invasive Methods of Diagnosis and Treatment of Urological Diseases);
Leading Researcher, Medical Research and Education Centerб,
Moscow
D. V. Ergakov
Russian Federation
Dmitry V. Ergakov — M.D., Cand.Sc. (Med); Assoc.Prof., Dept. of Urology and Andrology;
Urologist, Urology Division (Minimally Invasive Methods of Diagnosis and Treatment of Urological Diseases),
Moscow
K. A. Asliev
Russian Federation
Kamol A. Asliev — M.D.; Urologist, Urology Division (Minimally Invasive Methods of Diagnosis and Treatment of
Urological Diseases),
Moscow
N. A. Baykov
Russian Federation
Nikolay A. Baykov — M.D.; Head, Urology Division,
Moscow
Review
For citations:
Martov A.G., Ergakov D.V., Asliev K.A., Baykov N.A. Ejaculation-sparing enucleation of benign prostate hyperplasia: is it almost feasible? Urology Herald. 2023;11(1):59-69. (In Russ.) https://doi.org/10.21886/2308-6424-2023-11-1-59-69













































