Scroll to:
Multi-stage urethroplasy for anterior urethral strictures: objective parameters of long-term efficacy and patient-reported outcomes
https://doi.org/10.21886/2308-6424-2022-10-4-21-31
Abstract
Introduction. Multi-stage urethral surgery is used in cases of the most complex urethral strictures. The evaluation of surgical treatment results given by patients is a significant criterion for the efficacy of urethroplasty along with the assessment of urethral patency through instrumental examinations.
Objective. To evaluate the long-term efficacy of multistage urethroplasty for complex anterior urethral strictures considering the patients' quality of life and satisfaction with the surgical outcomes.
Materials and methods. The study included 73 patients aged 18 – 84 years with anterior urethral strictures who underwent multi-stage urethroplasty in 2010 – 2019. Surgical and functional outcomes of urethroplasty were assessed through general blood and urine tests, physical examination, uroflowmetry, and retrograde urethrography and urethroscopy in case of urinary disorders. Subjective parameters of treatment efficacy were studied using questionnaires: International Prostate Symptom Score (IPSS); Quality of life (QoL); Patient-reported Outcome Measure for Urethral Stricture Surgery (USS-PROM); Patient Global Impression of Improvement (PGI-I).
Results. Recurrent urethral stricture was detected in 19 (26,0%) patients with the average follow-up period being 65 months. Independent urination was restored in 71 (97.3%) cases, including repeated interventions. After surgery, there was a significant increase in urinary flow rate parameters (Q max: 8.1 vs 19.1 ml/s, p < 0.0001; Q ave: 5.5 vs 10.7 ml/s; p = 0.0004), decrease in residual urine volume (62.4 vs 18.6 ml, p < 0.0001), decrease in total IPSS score (18.7 vs 5.7 points; p < 0.0001) and QoL index (4.3 vs 1 .8 points, p < 0.0001). A comparative analysis of preoperative and postoperative USS-PROM questionnaire results demonstrated an improvement in indicators assessing LUTS (12.9 vs 3.4 points; p < 0.0001; 3.6 vs 1.7 points; p < 0.0001), and urination-associated quality of life (2.6 vs 0.6 points; p < 0.0001) and overall health (EQ-5D index: 0.73 vs 0.91 points; p = 0.025; EQ-VAS: 68.0 vs 88.1 points, p = 0.004). Fifty-seven (81.4%) men were “very satisfied” or “satisfied” with the treatment outcomes, while nine (12.9%) respondents noted a moderate effect of residual urinary disorders on the quality of life. Significantly higher satisfaction was observed among cystostomy patients and in cases where repeated interventions were unnecessary.
Conclusion. Multi-stage urethroplasty for complex anterior urethral strictures achieves efficacy in 97.3% of cases and is accompanied by high levels of quality of life and patient’s satisfaction during long-term follow-up.
For citations:
Glukhov V.P., Ilyash A.V., Vasilev K.S., Slyusarenko N.V., Ismailov R.S., Mitusov V.V., Sizyakin D.V., Kogan M.I. Multi-stage urethroplasy for anterior urethral strictures: objective parameters of long-term efficacy and patient-reported outcomes. Urology Herald. 2022;10(4):21-31. (In Russ.) https://doi.org/10.21886/2308-6424-2022-10-4-21-31
Introduction
Throughout the history of reconstructive urology, multiple augmentation, and replacement urethroplasty techniques have been proposed. All of them are aimed at achieving a single goal: restoration of urethral integrity, which will ensure unimpeded urine outflow from the bladder while maintaining an acceptable QoL (QoL) with minimal undesirable consequences [1][2].
However, until recently, the major criterion for the effectiveness of urethroplasty was only the assessment of urethral patency by instrumental examinations, while patients' assessment of treatment outcomes was not given proper attention [1][3][4]. The focus of modern urethral surgery development is related to the personalization of surgical techniques, and often with high awareness, the choice of a treatment technique is left to the patient. The authors believe that patient satisfaction of expectations from urethroplasty goes beyond “technical results” and the indicator of QoL and, as a result, overall patient satisfaction with urethroplasty results becomes a significant criterion of treatment effectiveness. Furthermore, subjective feelings of patients and various symptoms are equally important, if not more, factors in patient satisfaction, which must also be considered in evaluating the success of urethroplasty [5–8].
Patients with extended, panurethral, or multifocal urethral strictures after multiple ineffective endoscopic and open interventions in history, including hypospadias, as well as men with inflammatory strictures associated with lichen sclerosus or post-radiation constrictions, have the least favorable prognosis to achieve high urethroplasty efficiency rates [9]. As a rule, such patients have poor urethral plate quality, massive spongiofibrosis, and scar changes in the surrounding tissues, which require complete or partial excision and a staged treatment approach [10].
The study aimed to evaluate the long-term efficacy of multistage urethroplasty for complex anterior urethral strictures considering the QoL of patients and the satisfaction with the surgical outcomes.
Materials and methods
Study design. The data of 754 patients operated in the Urology Division, the Rostov State Medical University Clinic in 2010–2019 for urethral strictures were prospectively collected in an electronic database and retrospectively studied after the approval of the local independent ethics committee (Protocol No. 13/21 dated September 9, 2021). The criterion for inclusion of patients in the study was a combination of three clinical factors: 1) age of the patients, 18 years old or older; 2) localization of strictures in the spongy urethra; and 3) type of surgery – multistage urethroplasty. Exclusion criteria were proximal urethral strictures (membranous, prostatic), stenoses of the urethrovesical anastomosis and bladder neck, previously untreated congenital anomalies (hypospadias and epispadias) and any other urethral operations that did not meet the inclusion criteria, and incomplete multistage urethroplasty. Therefore, 73 patients were selected for the study. The primary endpoints of the study were the evaluation of the development of stricture recurrence. Secondary endpoints were the assessment of functional outcomes of urethroplasty, QoL, and patient satisfaction.
Pre-operative examination. All patients underwent a standard preoperative examination that included laboratory blood and urine tests, physical examination, ultrasound of the urinary system, urethrocystography, and cystoscopy to assess the extent, localization, and degree of stricture narrowing. In patients with preserved urinary continence (n = 54), the urination rate and the post-void residual urine volume (PVR), and the severity of lower urinary tract symptoms (LUTS) were examined by the International Prostate Symptom Score (IPSS), including the QoL scale for Urinary Disorders (QoL). Patients operated in 2015–2019 (n = 33) additionally completed the Patient-reported Outcome Measure for Urethral Stricture Surgery (USS-PROM) questionnaire.
Surgical techniques. Staged skin (26 (36.0%)) and buccal (47 (64.0%)) graft urethroplasty techniques were used [11]. Two-stage surgery was performed in 57 (78.0%) cases; surgeries with over two stages were performed in 16 (22.0%) patients. Complete excision and replacement of the affected urethral plate were required in 8 (11.0%) cases; urethral augmentation was performed in 65 (89.0%) observations. The time intervals between the first stage and subsequent stages ranged from 2 to 38 months; on average, surgical treatment took 10.97 ± 8.59 (2 to 57) months.
Objective evaluation. The evaluation of surgical and functional outcomes of multistage urethroplasty was designed as an observational study. The development of disease recurrence was evaluated based on examinations performed 3, 6, and 12 months after surgery during the first year of monitoring and then annually. If necessary, the patients visited the clinic beyond the scheduled follow-up period. Monitoring included standard laboratory tests of blood and urine, physical examination, and uroflowmetry. Retrograde urethrography and urethroscopy were performed to assess the causes of obstructive micturition if urinary disorders were detected. The level of Q max > 10 ml/s and PVR ≤ 50 ml, as well as the absence of radiological signs of urethral constriction and the need for unplanned interventions (dilation, catheterization, surgery) were considered satisfactory by objective parameters of surgical treatment. The evaluation of the treatment results included the data from the examinations of the last visit. The average follow-up period was 65.0 ± 30.9 (13–130) months.
Subjective evaluation. The study of subjective evaluations of symptoms, QoL, and patient satisfaction with surgery outcomes was designed as a cross-sectional study. The data were analyzed at one time point in different periods of postoperative follow-up. The mean period from surgery to the questionnaire survey was 67.8 ± 32.3 (14 to 134) months. Patients filled out printed versions of the questionnaires independently during a routine examination in the clinic or sent the completed forms by e-mail. From the total number of patients, 68 (93.2%) respondents participated in the postoperative questionnaire survey using IPSS-QoL, and 70 (95.9%) men completed the USS-PROM and the Patient Global Impression of Improvement scale (PGI-I).
LUTS severity during preoperative and postoperative periods was studied based on the results of the IPSS questionnaire. The total IPSS score could range from 0 to 35, with the most severe symptoms being indicated by a score of 35. The QoL scale was divided into 3 categories, with a QoL score of 0 → 2 representing satisfactory QoL, a QoL score of 3 representing acceptable QoL, and a QoL score of 4 → 6 representing unsatisfactory QoL.
Based on the results of the USS-PROM questionnaire survey, the authors additionally analyzed the subjective evaluation of LUTS (LUTS domain and visual-analog scale for assessment of urine flow – Peeling scale). The authors also studied the influence of symptoms on the QoL related to urination (QoL-LUTS block – Likert scale) and overall health (visual-analog scale for assessment of overall health – Euro-Qol-VAS scale and Euro-Qol-5D index). Patients who had a cystostomy drain or urethral catheter answered only the second part of the questionnaire, which included the Euro-Qol-VAS visual analogue scale and questions concerning mobility, self-care, daily activities, pain/discomfort, and anxiety/depression (Euro-Qol-5D index). The USS-PROM version of the postoperative assessment of men had two additional questions describing patients’ satisfaction with the results of treatment.
The PGI-I scale allowed patients to identify their current state of health compared to their preoperative state with a seven-point scale that ranged from 'much better' to 'much worse'.
Statistical analysis. Statistical data processing was performed using IBM SPSS Statistics 25.0 software (“SPSS: An IBM Company”, “IBM SPSS Corp.”, Armonk, NY, USA). The values were checked for normality of distribution using the Kolmogorov-Smirnov and Shapiro-Wilk tests. Descriptive analysis values were calculated. Relapse-free disease course functions and calculation of the cumulative probability of relapse development were studied using the Kaplan-Mayer test. Mean differences (Δ) and 95% confidence interval (95% CI) were calculated for pre- and postoperative assessments. Patients’ satisfaction with the surgical outcome was studied depending on such clinical parameters as age, body mass index, etiology, extent and localization of strictures, the presence of cystostomy, duration of disease, previous treatment (dilation, endoscopic and open urethral surgeries in the history), surgical complications, and stricture recurrence. Wilcoxon's sign-rank test, Student’s T test for independent samples, and Mann-Whitney U test were used for hypothesis testing. The accepted significance levels were p < 0.05 and p < 0.01 for a = 0.05 and a = 0.01.
Results
Patient characteristics. The mean age of the patients was 43.03 ± 15.31 (18 to 84) years old. Thirty-nine patients (53.4%) had penile strictures, 7 (9.6%) had bulbar, 15 (20.5%) had penile-bulbar, and 12 (16.4%) had multifocal strictures. The average length of the strictures was 7.27 ± 3.26 (2–18) cm. The duration of the disease was 7.87 ± 8.99 (0.25–45) years. Primary strictures were diagnosed in 25 (34.2%) patients, and 48 (65.8%) patients had various types of open and endoscopic interventions in the anamnesis, resulting in the disease recurrence. Among the strictures, those prevailed that developed because of iatrogenic (29 (39.7%)) and inflammatory (24 (32.9%)) lesions; traumatic strictures were revealed in 14 (19.2%) men, idiopathic – in 6 (8.2%). Natural urination was preserved in 54 (74.0%) patients, and 19 (26.0%) had cystostomy.
Surgical outcomes. Multistage surgery restored natural urination in 71 (97.3%) observations, including cases that required repeated surgical intervention to eliminate complications that developed at different times after intermediate stages of urethroplasty (25 (34.2%) patients) and stricture recurrence diagnosed after the final stage of urethroplasty (19 (26.0%) patients). Kaplan-Mayer survival analysis showed that the highest risk of recurrence was observed during the first months of the follow-up. The minimum cumulative probability of relapse is 0.7 and remains constant after 57 months of follow-up (Fig. 1).
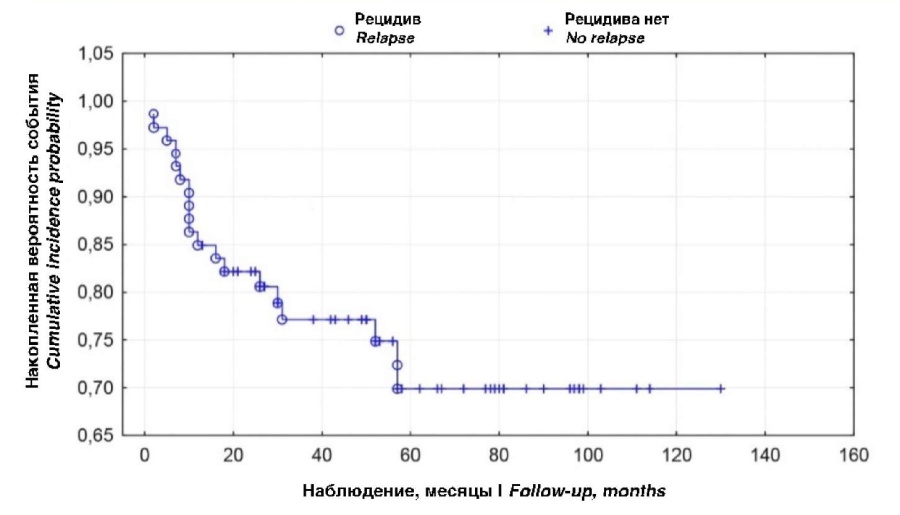
Figure 1. Timing of urethral recurrence according to Kaplan-Mayer multi-scoring for patients undergoing multistage urethroplasty
Functional results. The analysis of uroflowmetry data revealed a significant increase in postoperative urine flow rate parameters compared to preoperative values (Q max: 8.1 vs 19.1 ml/s, p < 0.0001; Q ave: 5.5 vs 10.7 ml/s; p = 0.0004) and a decrease in PVR (62.4 vs 18.6 ml, p < 0.0001) (Table 1).
Table 1. Uroflowmetry values and post-void residual urine volume
|
Characteristics |
Preoperative |
Postoperative |
p |
M difference |
95% CI for M difference |
|
M ± SD (max – min) |
|||||
|
Q max, ml/s |
8.14 ± 3.74 |
19.08 ± 2.65 |
< 0.0001 |
9.9 |
6.77 – 17.13 |
|
Q ave, ml/s |
5.45 ± 2.75 |
10.74 ± 1.96 |
0.0004 |
4.3 |
5.87 – 9.32 |
|
PVR, ml |
62.4 ± 55.6 |
18.6 ± 15.4 |
< 0.0001 |
-48.8 |
-89 – -10.27 |
Note. M — mean; SD — standard deviation; max – min — minimum and maximum values; CI — confidence interval; Q max — maximum urine flow rate; Q ave — average urine flow rate; PVR — post-void residual volume
Subjective results. IPSS-QoL questionnaire. The average total IPSS score decreased from 18.7 to 5.7, the QoL index – from 4.3 to 1.8 (Table 2). When the QoL index was divided into three categories, it was noted that before surgery, none of the patients considered their urinary-related QoL satisfactory (QoL index 0 → 2), 13.0% considered it acceptable (QoL index = 3), and 87.0% considered it unsatisfactory (QoL index 4 → 6). After surgical treatment, 85.3% rated their QoL as satisfactory, 14.7% acceptable, and none of the patients considered it unsatisfactory.
Table 2. IPSS and QoL scores
|
Characteristics |
Preoperative |
Postoperative |
p |
M difference |
95% CI for M difference |
|
M ± SD (max – min) score |
|||||
|
IPSS |
18.65 ± 5.90 |
5.26 ± 1.68 |
< 0.0001 |
-13.4 |
-17.4 – -6.3 |
|
QoL |
4.27 ± 1.26 |
1.78 ± 0.64 |
< 0.0001 |
-2.5 |
-3.7 – -1.9 |
Note. M — mean; SD — standard deviation; max – min — minimum and maximum values; CI — confidence interval; IPSS — International Prostate Symptom Score; QoL — QoL
USS-PROM questionnaire. A comparative analysis of the pre- and postoperative results of the USS-PROM questionnaire survey also demonstrated an improvement in the indicators assessing LUTS and QoL related to urination and overall health (Table 3).
Table 3. USS-PROM scores
|
Characteristics |
Preoperative |
Postoperative |
p |
M difference |
95% CI for M difference |
|
M ± SD (max – min) score |
|||||
|
LUTS* |
12.9 ± 3.45 |
3.4 ± 2.0 |
< 0.0001 |
-9.4 |
-10.1 – -6.2 |
|
Peeling’s picture* |
3.6 ± 0.43 |
1.7 ± 0.37 |
< 0.0001 |
-1.8 |
-1.9 – -1.3 |
|
LUTS-QOL* |
2.6 ± 0.67 |
0.6 ± 0.13 |
< 0.0001 |
-2.0 |
-2.4 – -1.9 |
|
Index EQ-5D |
0.73 ± 0.08 |
0.91 ± 0.12 |
0.025 |
0.2 |
20.8 – 27.3 |
|
EQ-VAS |
68.0 ± 5.89 |
88.1 ± 4.37 |
0.004 |
19.9 |
0.1 – 0.2 |
Note. n — number of patients; M — mean; S — standard deviation; max – min — minimum and maximum values; CI — confidence interval; LUTS — lower urinary tract symptoms; LUTS-QOL — LUTS-specific QoL(Likert scale); EQ-5D — EuroQol-5 dimension; EQ-VAS — EuroQol-visual analog scales
* Includes only patients who had natural urination preoperatively
The evaluation of satisfaction with the surgical outcomes showed that 57 (81.4%) patients were “very satisfied” (45.7%) or “satisfied” (35.7%) with the surgical outcome, 13 (18.6%) were “dissatisfied” (14.3%) or “not satisfied at all” (4.3%). The reason for dissatisfaction in six (8.6%) men was the emergence of new problems: post-micturition dribbling, angle curvature, and cosmetic defects of the penile skin with an overall improvement in quality of urination. Five (7.1%) men noted that the quality of their urination did not improve after surgery, and two (2.9%) patients considered that not only the quality of urination did not improve after surgery, but also new problems appeared. At the same time, a moderate negative impact of the symptoms of urinary dysfunction on the QoL was noted by 9 (12.9%) respondents.
Analysis of the relationship between patients' satisfaction with the surgery outcomes and various clinical parameters showed that cystostomy-patients were significantly more often “very satisfied” or “satisfied” with the result of multistage urethroplasty than those who could urinate naturally before surgery. Furthermore, the absence of surgical complications requiring repeated urethral surgery and/or permanent dilation was a significant predictor of positive satisfaction scores, while the presence of complications itself had no significant effect on satisfaction, nor did the presence of recurrence (Table 4).
Table 4. Relationship between patients’ satisfaction with the surgery outcomes and selected clinical parameters
|
Characteristics |
“Very satisfied” or “Satisfied” |
“Unsatisfied” or “Very unsatisfied” |
p |
|
Cystostomy |
|||
|
No |
39 (76.5%) |
12 (23.5%) |
0.02 |
|
Yes |
18 (94.7%) |
1 (5.3%) |
|
|
Complications |
|||
|
No |
31 (88.6%) |
4 (11.4%) |
0.114 |
|
Yes |
26 (74.3%) |
9 (25.7%) |
|
|
Surgery for complications |
|||
|
No |
12 (52.2%) |
11 (47.8%) |
0.004 |
|
Yes |
45 (95.7%) |
2 (4.3%) |
|
|
Stricture recurrence |
|||
|
No |
46 (88.5%) |
6 (11.5%) |
0.062 |
|
Yes |
11 (61.1%) |
7 (38.9%) |
|
Note. n — number of patients
PGI-I scale. The answers of patients who completed the PGI-I scale showed that their overall condition after surgery compared to what it was before surgery became “much better” in 34 (48.6%) cases, “a lot better” in 19 (27.1%), “slightly better” in 10 (14.3%), remained “no change” in 4 (5.7%), became “slightly worse” in 3 (4.3%), and none of the patients indicated that the condition became “much worse” or “significantly worse”.
Discussion
The definition of what constitutes a successful urethroplasty varies widely in the publications [1]. Traditionally, the perspective of a 'successful' urethroplasty has been that no repeat surgery and/or permanent dilation is necessary. Over 75% of the publications issued between 2000 and 2008 contain this definition as the main interpretation of the effectiveness of urethroplasty, largely due to the simplicity of quantification [12]. However, this definition does not include the functional results of surgery and the assessments made by patients, including QoL related to health related to health generally and urination particularly. For example, there are known cases when after urethroplasty, patients experienced significant anxiety due to urinary leakage or persistent dysuria and were generally dissatisfied with their surgical experience but had no anatomical narrowing of the urethra or need for repeated intervention.
Another common non-invasive method of assessing and monitoring the results of urethroplasty is uroflowmetry [3]. However, urinary velocity parameters have never been used as an independent tool for screening the stricture recurrence and, as a rule, require additional assessment with the use of radiological and endoscopic tests. Morey et al. (1998) were the first to use uroflowmetry and retrograde urethrography data in correlation with the American Urological Association Symptom Score (AUA-SS), also known as the IPSS questionnaire. In patients with radiological signs of successful urethral reconstruction, the authors observed a significant reduction in the total AUA-SS score (26.9 vs 5.1; p < 0.0001) and an inverse correlation between the AUA-SS score and the maximum urine flow rate (r = -0.712; p < 0.0001), concluding that the total AUA-SS symptoms score had clinical validity as an additional assessment tool for urethroplasty results [13].
Subsequenty, the AUA-SS or IPSS questionnaires became widely used in many studies investigating the functional aspects of urethral surgery, but designed specifically for patients with prostatic hyperplasia, it does not adequately assess all symptoms due to urethral stricture, despite their obvious similarities. Thus, Nuss et al. (2012) found that in patients with urethral strictures, up to 21% of symptoms were not detected during the questionnaire survey with the IPSS questionnaire [14].
The first validated questionnaire developed for men who underwent surgical treatment for anterior urethral strictures was presented in 2011 by a group of scientists from the UK and was called Patient-reported Outcome Measure for Urethral Stricture Surgery (USS-PROM) [15]. This questionnaire allows for the evaluation of the effectiveness of urethroplasty from the patients' point of view, expressing in quantitative (point) equivalent their subjective perception regarding not only the disease symptoms but also the QoL related to urination and overall health level, as well as treatment satisfaction.
Currently, the questionnaire has versions in various languages of the world and is used in many countries. In Russia, a group of researchers from Vladimirsky Moscow Regional Clinical Research Institute conducted an ethnolinguistic adaptation of the Russian version of the USS-PROM questionnaire in 2015 [16]. Subsequently, the authors published a study on the evaluation of the efficacy of various surgical treatment methods of anterior urethral strictures based on the evaluations provided by the patients when completing a USS-PROM questionnaire [17]. In the total group of patients, regardless of urethroplasty techniques, the mean value of the LUTS domain after surgical treatment was 7.4 points and the Peeling's scale index was 2.3 points. The present study showed more favorable symptoms severity scores (3.4 and 1.7) compared to the data of Russian colleagues [17] and was comparable with the results of the questionnaire authors — 3.0 and 1.8 points, respectively [15]. 11% and 19% of the patients in the Russian and British studies observed a moderate or strong negative impact of residual urinary tract symptoms on QoL. The lowest Euro-Qol-VAS scale score and the Euro-Qol-5D index score were observed in the Russian study (73 and 0.79 points), the highest — in the present study (88.1 and 0.91 points). British patients rated their health status on the Euro-Qol-VAS scale at 81 points, and their Euro-Qol-5D index score was 0.87. However, the satisfaction of the patients in the present study who underwent exclusively multistage urethroplasty was slightly lower (81.4%) compared to the observational series of Shibaev et al. (2016) and Jackson et al. (2011), wherein it was 86.7% and 96.0%, respectively, and referred to various techniques of urethral surgery from endoscopic to buccal-graft urethroplasty [15][17]. It can be assumed that this is associated with a greater number of complications and recurrences observed in patients with complicated strictures or are caused by the duration of treatment.
Therefore, the trends in the development of the concept of urethral surgery efficacy reveal the increasing importance of the subjective component, which allows the specialists to significantly complement the objective picture of the patient's disease and condition during treatment and the screening for stricture recurrence. Any urethroplasty should ultimately improve patients’ overall QoL, and high urethroplasty efficacy is a balance between meeting patients’ expectations and perceptions and what surgeons consider to be a surgical success.
Conclusion
Multistage augmentation and replacement urethroplasties for complex anterior urethral strictures are effective in 97.3% of cases according to objective parameters and are accompanied by high levels of QoL and patient satisfaction during long-term follow-up.
References
1. Lucas ET, Koff WJ, Rosito TE, Berger M, Bortolini T, Neto BS. Assessment of satisfaction and Quality of Life using self -reported questionnaires after urethroplasty: a prospective analysis. Int Braz J Urol. 2017;43(2):304-310. https://doi.org/10.1590/S1677-5538.IBJU.2016.0207
2. Bertrand LA, Voelzke BB, Elliott SP, Myers JB, Breyer BN, Vanni AJ, McClung CD, Tam CA, Warren GJ, Erickson BA; Trauma and Urologic Reconstruction Network of Surgeons. Measuring and Predicting Patient Dissatisfaction after Anterior Urethroplasty Using Patient Reported Outcomes Measures. J Urol. 2016;196(2):453-61. https://doi.org/10.1016/j.juro.2016.01.117
3. Erickson BA, Breyer BN, McAninch JW. The use of uroflowmetry to diagnose recurrent stricture after urethral reconstructive surgery. J Urol. 2010;184(4):1386-90. https://doi.org/10.1016/j.juro.2010.06.015
4. Yeung LL, Brandes SB. Urethroplasty practice and surveillance patterns: a survey of reconstructive urologists. Urology. 2013;82(2):471-5. https://doi.org/10.1016/j.urology.2013.03.069
5. Amirbekov B.G., Kogan M.I., Mitusov V.V., Mirzayev Z.A., Kosterov M.V. Quality of life dynamics in men after urethral stricture surgery. Vestnik Urologii. 2019;7(2):5-13. (In Russ.) https://doi.org/10.21886/2308-6424-2019-7-2-5-13
6. Vetterlein MW, Gödde A, Zumstein V, Gild P, Marks P, Soave A, Meyer CP, Riechardt S, Dahlem R, Fisch M, Kluth LA; Trauma and Reconstructive Urology Working Party of the European Association of Urology Young Academic Urologists. Exploring the intersection of functional recurrence, patient-reported sexual function, and treatment satisfaction after anterior buccal mucosal graft urethroplasty. World J Urol. 2021;39(9):3533-3539. https://doi.org/10.1007/s00345-021-03648-y
7. Redmond E, Bekkema J, Rourke K. Comprehensive Prospective Assessment of Patient-reported Outcomes Following Urethroplasty. Urology. 2020;141:162-167. https://doi.org/10.1016/j.urology.2020.02.034
8. Usupbaev A.C., Kurbanaliev R.M., Akylbek S., Stambekova K.N., Mukanbaev K. Urethral strictures caused by lichen sclerosus: evaluation of patient quality of life after buccal urethroplasty. Vestnik Urologii. 2022;10(2):78-86. (In Russ.) https://doi.org/10.21886/2308-6424-2022-10-2-78-86
9. Kogan M.I., Glukhov V.P., Ilyash A.V., Mitusov V.V., Chibichyan M.B. Complex spongy urethral strictures with multistage treatment: predicting the recurrence risk. Experimental and Clinical Urology, 2022;15(1):136-141. (In Russ.) https://doi.org/10.29188/2222-8543-2022-15-1-136-141
10. Lumen N., Campos-Juanatey F., Dimitropoulos K., Green-well T., Martins F.E., Osman N., Riechardt S., Waterloos M. Urethral Strictures In: EAU Guidelines. Edn. presented at the EAU Annual Congress Amsterdam 2022. ISBN 978-94-92671-16-5. EAU Guidelines Office, Arnhem, the Nether-lands, 2022. https://uroweb.org/guidelines/urethral-strictures
11. Glukhov V.P., Kogan M.I., Ilyash A.V., Bugaenko V.A. Comparative analysis of patients with spongy urethral strictures undergoing multistage urethroplasty or permanent urethrostomy. Urologiia. 2022;(4):10-14. (In Russ.) https://dx.doi.org/10.18565/urology.2022.4.10-14
12. Meeks JJ, Erickson BA, Granieri MA, Gonzalez CM. Stricture recurrence after urethroplasty: a systematic review. J Urol. 2009;182(4):1266-70. https://dx.doi.org/10.1016/j.juro.2009.06.027
13. Morey AF, McAninch JW, Duckett CP, Rogers RS. American Urological Association symptom index in the assessment of urethroplasty outcomes. J Urol. 1998;159(4):1192-4. PMID: 9507830
14. Nuss GR, Granieri MA, Zhao LC, Thum DJ, Gonzalez CM. Presenting symptoms of anterior urethral stricture disease: a disease specific, patient reported questionnaire to measure outcomes. J Urol. 2012;187(2):559-62. https://dx.doi.org/10.1016/j.juro.2011.10.043
15. Jackson MJ, Sciberras J, Mangera A, Brett A, Watkin N, N'dow JM, Chapple CR, Andrich DE, Pickard RS, Mundy AR. Defining a patient-reported outcome measure for urethral stricture surgery. Eur Urol. 2011;60(1):60-8. https://dx.doi.org/10.1016/j.eururo.2011.03.003
16. Bazaev V.V., Shibaev A.N., Pavlova Yu.V. Validation of the Russian Version of the Questionnaire to Assess the Effectiveness of Surgical Treatment of Patients with Anterior Urethral Stricture (Patient-Reported Outcome Measure for Urethral Stricture Surgery (PROM-USS): a Pilot Study. Urologiia. 2015;5:15-21. (In Russ.) EDN: UYMTNB
17. Shibaev A.N., Bazaev V.V., Pavlova Yu.V. Quality of life as an effectiveness criterion of surgical treatment for anterior urethral strictures. Urologiia. 2016;5:32-36. (In Russ.) EDN: XBKFGJ
About the Authors
V. P. GlukhovRussian Federation
Vladimir P. Glukhov — M.D., Cand.Sc.(Med), Assoc.Prof. (Docent), Assoc.Prof., Dept. of Urology and Human Reproductive Health (with the Pediatric Urology and Andrology Сourse), Rostov State Medical University.
29 Nakhichevanskiy Ln., Rostov-on-Don, 344022
Competing Interests:
The authors declare no conflicts of interest
A. V. Ilyash
Russian Federation
Anna V. Ilyash — M.D., Cand.Sc.(Med), Assist.Prof., Dept. of Urology and Human Reproductive Health (with the Pediatric Urology and Andrology Course), Rostov State Medical University.
29 Nakhichevanskiy Ln., Rostov-on-Don, 344022
Competing Interests:
The authors declare no conflicts of interest
K. S. Vasilev
Russian Federation
Kirill S. Vasilev — Resident, Rostov State Medical University.
29 Nakhichevanskiy Ln., Rostov-on-Don, 344022
Competing Interests:
The authors declare no conflicts of interest
N. V. Slyusarenko
Russian Federation
Nikita V. Slyusarenko — Resident, Rostov State Medical University.
29 Nakhichevanskiy Ln., Rostov-on-Don, 344022
Competing Interests:
The authors declare no conflicts of interest
R. S. Ismailov
Russian Federation
Ruslan S. Ismailov - M.D., Cand.Sc.(Med), Assist.Prof., Dept. of Urology and Human Reproductive Health (with Pediatric Urology and Andrology Course), Rostov State Medical University.
29 Nakhichevanskiy Ln., Rostov-on-Don, 344022
Competing Interests:
The authors declare no conflicts of interest
V. V. Mitusov
Russian Federation
Valeriy V. Mitusov — M.D., Dr.Sc.(Med), Assoc.Prof. (Docent), Prof., Dept. of Urology and Human Reproductive Health (with the Pediatric Urology and Andrology Сourse), Rostov State Medical University.
29 Nakhichevanskiy Ln., Rostov-on-Don, 344022
Competing Interests:
The authors declare no conflicts of interest
D. V. Sizyakin
Russian Federation
Dmitriy V. Sizyakin — M.D., Dr.Sc.(Med), Full Prof., Prof., Dept. of Urology and Human Reproductive Health (with the Pediatric Urology and Andrology course), Rostov State Medical University.
29 Nakhichevanskiy Ln., Rostov-on-Don, 344022
Competing Interests:
The authors declare no conflicts of interest
M. I. Kogan
Russian Federation
Mikhail I. Kogan — M.D., Dr.Sc.(Med), Full Prof., Honored Scientist of the Russian Federation, Head, Dept. of Urology and Human Reproductive Health (with Pediatric Urology and Andrology Course), Rostov State Medical University.
29 Nakhichevanskiy Ln., Rostov-on-Don, 344022
Competing Interests:
The authors declare no conflicts of interest
Review
For citations:
Glukhov V.P., Ilyash A.V., Vasilev K.S., Slyusarenko N.V., Ismailov R.S., Mitusov V.V., Sizyakin D.V., Kogan M.I. Multi-stage urethroplasy for anterior urethral strictures: objective parameters of long-term efficacy and patient-reported outcomes. Urology Herald. 2022;10(4):21-31. (In Russ.) https://doi.org/10.21886/2308-6424-2022-10-4-21-31













































