Scroll to:
Efficacy of a synthetic middle urethral sling in patients with mixed urinary incontinence
https://doi.org/10.21886/2308-6424-2022-10-2-53-62
Abstract
Introduction. Mixed urinary incontinence is believed to be more difficult to treat than stress urinary incontinence and overactive bladder (OAB) alone. However, the mixed form occurs in one in three women with complaints of incontinence. Therefore, the evaluation of the effectiveness of the transobturator suburethral sling in patients with a mixed form of urinary incontinence is a topical issue.
Objective. To evaluate the efficacy of the transobturator suburethral sling in patients with mixed urinary incontinence.
Materials and methods. The cohort study enrolled 106 patients with a mixed form of urinary incontinence. Validated questionnaires (Overactive bladder questionnaire/OABq, Urinary Distress Inventory, Short Form/UDI-6) were used to assess subjective data. Secondary endpoint – objective data of comprehensive urodynamic study 2 – 12 months after transobturator suburethral sling implantation: presence of phase, terminal, constrictor-induced detrusor overactivity (DOA).
Results. According to the preoperative evaluation of complaints on validated questionnaires, the mean UDI-6 score was 52.2 ± 16.3 points, OABq was 15.4 ± 5.4 points. After surgery, there was a decrease in the UDI-6 questionnaire scores to 19.4 ± 18.4 scores and OABq to 9.6 ± 4.1 scores, the difference for both of which was statistically significant (p < 0.001). Terminal DOA was sighted in 44 (41.5%) preoperative patients and 33 (31.1%) postoperative patients (p = 0.153). Stress-induced DOA was observed in 27 (25.5%) before and 6 (5.7%) after surgery (p < 0.001), respectively. Seventy-two (67.9%) patients reported satisfaction with the surgery and willingness to recommend it to their friends. For 26 (24.5%) patients, the surgery had no significant effect on quality of life. Eight (7.5%) patients noted a worsening of symptoms after treatment. No effect of sling installation on the course of OAB was found.
Conclusion. The placement of a synthetic suburethral sling has improved the quality of life in many patients with a mixed form of urinary incontinence.
For citations:
Zaitseva A.O., Volkova O.V., Labetov I.A., Kovalev G.V., Shkarupa D.D. Efficacy of a synthetic middle urethral sling in patients with mixed urinary incontinence. Urology Herald. 2022;10(2):53-62. (In Russ.) https://doi.org/10.21886/2308-6424-2022-10-2-53-62
Introduction
Urinary incontinence is a widespread disease registered in up to 58.0% of women [1]. More than half of patients have mixed urinary incontinence (MUI), which includes the symptoms of stress urinary incontinence (SUI) and overactive bladder (OAB). International Continence Society (ICS) defines MUI as a complaint of involuntary leakage of urine associated with urgency and also with exertion, effort, sneezing, or coughing and micturition urgency, frequent urination, and urge urinary incontinence [2]. According to the NHANES survey, which included data from 4,229 women older than 20 years old, this form is observed in every third woman with complaints of urinary incontinence [3]. It is believed that MUI is more difficult to treat than SUI and OAB alone [3-5]. First-line therapy can include behavioral therapy and pelvic muscle training that is followed by OAB pharmacotherapy and a combination of methods [6-9]. However, a lot of women must undergo surgical intervention for the repair of anatomic causes of SUI. There are still not enough data on the influence of the implantation of a transobturator suburethral sling on the course of OAB [6][7][9].
The study aimed to evaluate the effectiveness of a transobturator suburethral sling in patients with MUI.
Materials and methods
The study included women with MUI who underwent treatment at St. Petersburg University’s N.I. Pirogov Clinic of High Medical Technologies from 2017 to 2020. The mean age of women was 58.6 ± 0.4 years old. The stress component of urinary incontinence is verified based on a gynecological examination (cough stress test and Ulmsten probe). The presence of detrusor hyperactivity and urgent urinary incontinence was evaluated by a multichannel urodynamic study. The present study included invasive and non-invasive urodynamic methods of diagnostics: uroflowmetry, filling cystometry, and voiding cystometry (flow-pressure study).
Detrusor pressure values were obtained by a deduction of abdominal pressure from vesical pressure. Vesical pressure was measured with a water-perfusion urodynamic catheter 8 Fr (Laborie Medical Technologies Inc., Mississauga, ON, Canada) installed in the bladder lumen. Abdominal pressure was measured with a water-perfusion urodynamic catheter 10 Fr (Laborie Medical Technologies Inc., Mississauga, ON, Canada) installed vaginally or rectally. The calibration of the values obtained was performed with a cough stress test before filling the cystometry (vesical and abdominal pressure values were identical). According to ICS, an elevation of the detrusor pressure in the filling phase is defined as detrusor overactivity (DOA). Phase DOA is a wavelike elevation of pressure during the rest period with/without the leakage of urine (Fig. 1). Stress-induced DOA (Fig. 2) is a wave-like elevation of pressure with/without the urine leakage in response to a cough stress test. Terminal DOA (Fig. 1) is an elevation of pressure with uncontrolled bladder emptying. After the verification of the diagnosis, all patients underwent standard implantation of a transobturator suburethral sling.
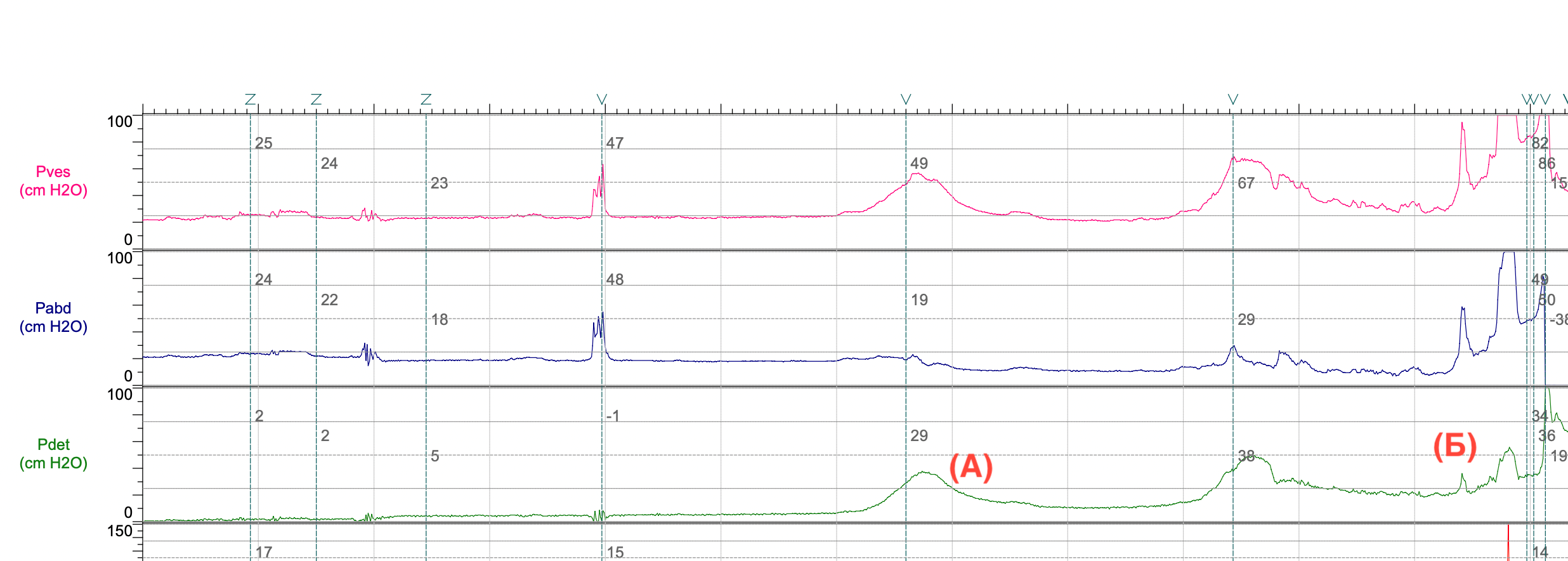
Figure 1. Fragment of multichannel urodynamic testing results: A — phase detrusor overactivity; B — terminal detrusor overactivity
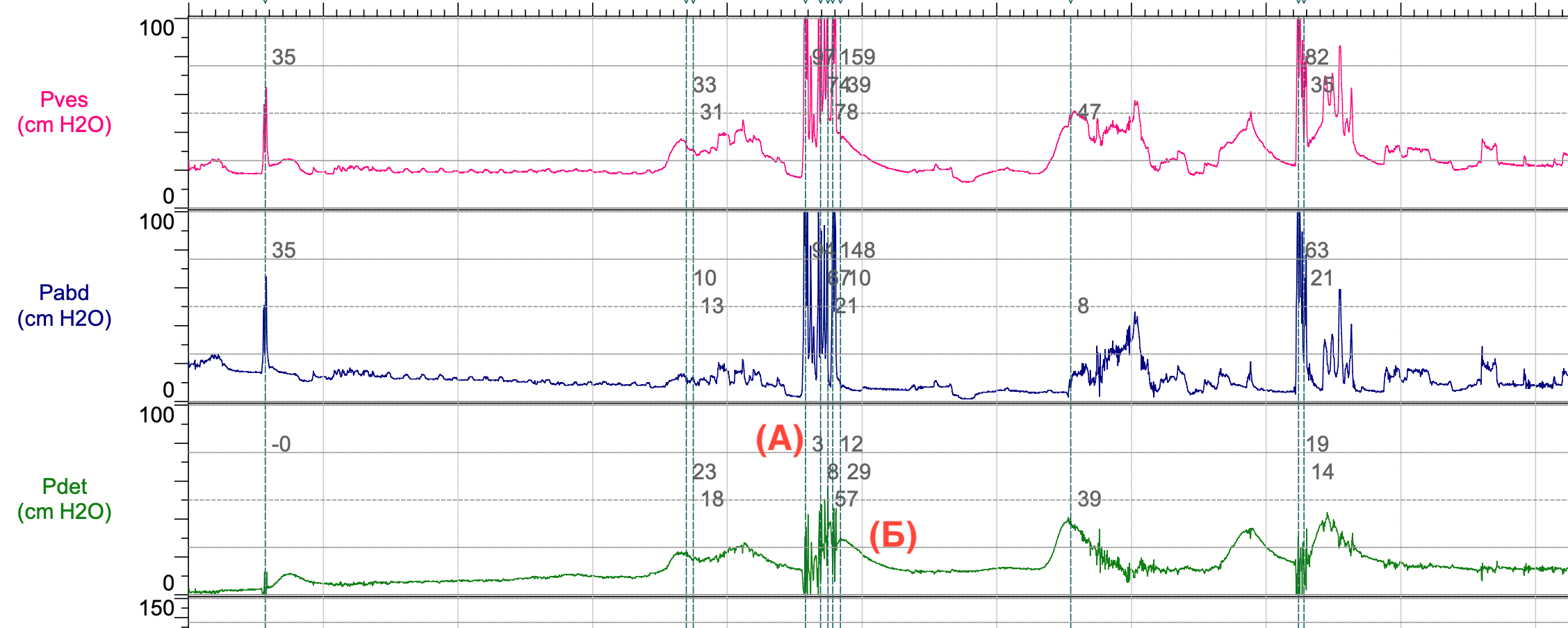
Figure 2. Fragment of multichannel urodynamic testing results: A — cough; B — stress-induced detrusor overactivity
Study design. This is retrospective cohort study. The patients’ data were collected from medical records with the further formation of a database. The first endpoint was a subjective evaluation of the efficiency of surgical treatment for MUI. Subjective data were evaluated with validated questionnaires (Overactive Bladder Questionnaire (OABq) and Urinary Distress Inventory, Short Form (UDI-6)). The secondary endpoint was objective data obtained from a complex urodynamic study 2 – 12 months after the implementation of a transobturator suburethral sling: the presence of phase, terminal, and stress-induced DOA.
Statistical analysis. Qualitative variables were described with the mean ± standard deviation and categorical variables were described with absolute numbers and percentages. Quantitative data was compared before and after treatment with the Wilcoxon test for associated samples. Cohort analysis was performed with Kruskal-Wallis ranks. Category features were analyzed with a precise Fisher’s test. The difference was statistically significant at p < 0.05. The calculations were made in the R version 4.1.3 programming language (The R Foundation for Statistical Computing, Vienna, Austria) [10].
Results
The study included 106 patients who met the study entry criteria.
Subjective results. The study of complaints before and after surgery using data from validated questionnaires showed that the mean UDI-6 score was 52.2 ± 16.3, the OABq score was 15.4 ± 5.4. After surgery, there was a decrease in the UDI-6 score to 19.4 ± 18.4 and the OABq score to 9.6 ± 4.1; the difference was statistically significant at (p < 0.001) in both (Fig. 3). Seventy-two (67.9%) women were satisfied with the surgical outcome. Twenty-six women (24.5%) said that their quality of life did not change significantly. Eight (7.5%) women said that the symptoms worsened after the treatment (Table 1).
Table 1. Subjective results
|
Indicator |
Feeling better (n = 72) |
No change (n = 26) |
Feeling worse (n = 8) |
p |
|
Age, years |
57 ± 11 |
62 ± 8 |
64 ± 9 |
0.040 |
|
Height, cm |
1.63 ± 0.06 |
1.63 ± 0.06 |
1.65 ± 0.09 |
0.6 |
|
Weight, kg |
78 ± 16 |
78 ± 15 |
95 ± 16 |
0.014 |
|
BMI, kg/m2 |
29.3 ± 5.2 |
29.4 ± 5.5 |
35.1 ± 6.1 |
0.016 |
|
UDI-6, points |
54 ± 16 |
50 ± 15 |
43 ± 18 |
0.2 |
|
OAB, points |
15.7 ± 5.2 |
13.5 ± 5.1 |
18.9 ± 6.4 |
0.029 |
|
Notes. BMI – body mass index; OABq – Overactive Bladder questionnaire; UDI-6 – Urinary Distress Inventory, Short Form |
||||
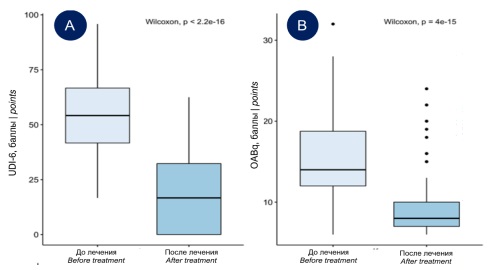
Figure 3. Data on the subjective evaluation of therapy effectiveness: A — evaluation according to the Urinary Distress Inventory, Short Form (UDI-6); B — evaluation according to the Overactive Bladder questionnaire (OABq)
Objective results. According to the results of the multichannel urodynamic study, there were changes in the functional parameters of the bladder before and after surgery. The first sensation of bladder filling in patients was at the volume of 80.3 ± 57.6 ml, and after the treatment, it was 90.7 ± 37.8 ml. These differences were statistically significant (p < 0.001). The volume of the first desire also changed from 147.1 ± 86.5 ml to 158.8 ± 53.3 ml (p = 0.007). Before the treatment, strong desire appeared at 305.2 ± 106.0 ml, and after the treatment, it did not change (313.3 ± 62.5 ml; p = 0.189). The maximum cystometric capacity was 399.2 ± 126.0 and 411.6 ± 93.3 ml, respectively (p = 0.002). The maximum flow rate changed from 30.4 ± 12.4 ml to 24.6 ± 9.7 ml (p < 0.001), the mean flow rate did not change (before the treatment — 12.9 ± 5.6 ml/s; after treatment — 12.2 ± 5.3 ml/s; p = 0.17). Before surgery, the maximum detrusor pressure was 31.8 ± 12.7 mmAq, after surgery — 25.8 ± 5.5 mmAq (p < 0.001). Detrusor pressure achieved at maximum urine flow (Pdet@Qmax) was 26.4 ± 9.3 and 24.5 ± 5.1 mmAq before and after surgery (p = 0.057), respectively (Figure 4). After treatment, the urination volume was 333.4 ± 109.8 ml. The post-void residual volume did not change (before the treatment — 2.9 ± 9.6 ml; after the treatment — 3.2 ± 13.2 ml; p = 0.663).
Phase DOA was observed in 70 (66.0%) patients. After the surgery, this condition was registered in 38 (35.8%) patients (p < 0.001). Before the surgery, terminal overactivity was observed in 44 (41.5%) patients; after the surgery, it was observed in 33 (31.1%) patients (p = 0.153). Stress-induced bladder overactivity was observed in 27 (25.5%) patients before surgery; and in 6 (5.7%) patients after surgery (p < 0.001). The surgery also affected the change in bladder compliance. Low compliance was observed in 32 patients (30.2%). After the surgery, it was observed in 27 patients (25.5%) (p = 0.54) (Table 2).
Тable 2. Objective results
|
Indicator |
Feeling better (n = 72) |
No change (n = 26) |
Feeling worse (n = 8) |
p |
|
Phase DOA, n (%) |
|
|
|
0.001 |
|
Yes |
19 (26) |
12 (46) |
7 (88) |
|
|
No |
53 (74) |
14 (54) |
1 (12) |
|
|
Terminal DOA, n (%) |
|
|
|
0.057 |
|
Yes |
18 (25) |
13 (50) |
2 (25) |
|
|
No |
54 (75) |
13 (50) |
6 (75) |
|
|
Stress-induced DOA, n (%) |
|
|
|
0.600 |
|
Yes |
4 (5,6) |
1 (3,8) |
1 (12) |
|
|
No |
68 (94) |
25 (96) |
7 (88) |
|
|
Low compliance, n (%) |
|
|
|
0.200 |
|
Yes |
19 (26) |
8 (31) |
0 (0) |
|
|
No |
53 (74) |
18 (69) |
8 (100) |
|
|
|
||||
|
First sensation, ml |
94 ± 37 |
85 ± 42 |
78 ± 32 |
0.400 |
|
First desire, ml |
162 ± 49 |
161 ± 66 |
126 ± 33 |
0.200 |
|
Strong desire, ml |
316 ± 53 |
316 ± 84 |
276 ± 57 |
0.200 |
|
Maximum capacity, ml |
421 ± 84 |
403 ± 116 |
351 ± 71 |
0.110 |
|
|
||||
|
pDet-max, mmH20 |
25.4 ± 5.1 |
25.5 ± 5.5 |
30.1 ± 7.2 |
0.064 |
|
pDet@Qmax, mmH20 |
24.5 ± 5.4 |
24.1 ± 4.5 |
26.1 ± 5.1 |
0.600 |
|
Qmax, ml/sec |
26 ± 10 |
22 ± 8 |
18 ± 5 |
0.042 |
|
Qaver, ml/sec |
12.8 ± 5.5 |
11.5 ± 4.6 |
8.5 ± 3.4 |
0.065 |
|
Post-void residual, ml |
3 ± 13 |
3 ± 14 |
8 ± 16 |
0.500 |
|
Urination volume, ml |
347 ± 119 |
318 ± 84 |
261 ± 63 |
0.079 |
|
Notes. DOA – detrusor overactivity; pDet@Qmax – detrusor pressure achieved at maximum urine flow; pDet-max – maximum detrusor pressure |
||||
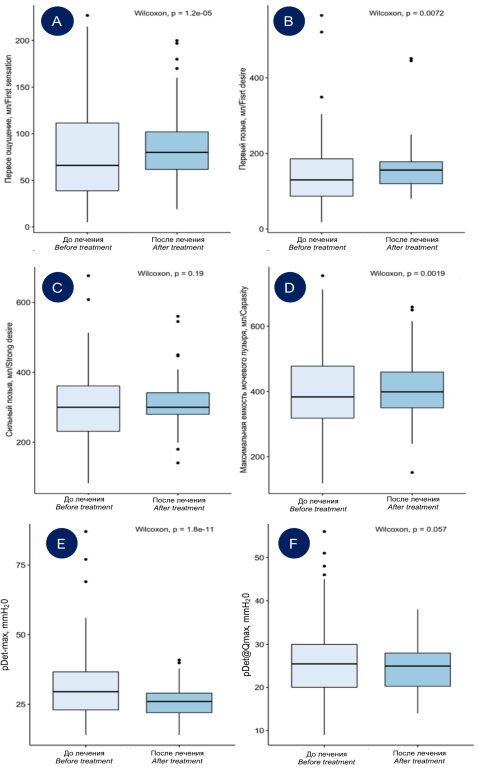
Figure 4. Data on shifts in urodynamic parameters during cystometry before and after surgery — bladder sensitivity and volume, detrusor pressure: A — first sensation; B — first desire; C — strong desire; D — maximum bladder capacity; E — maximum detrusor pressure (pDet-max); F — detrusor pressure achieved at maximum urine flow (pDet@Qmax)
Discussion
MUI remains an understudied and controversial issue in modern urogynecology. Since there are not enough data on the pathophysiology of the disease, the treatment cannot be standardized [11]. Currently, the diagnostics of MUI are based on the symptoms and objective results of the urodynamic study. Depending on the predominant form of urine incontinence, the tactics of treatment can vary. Patients with the prevalence of an urgent component of urinary incontinence receive the first-line therapy that includes behavioral therapy, pelvic muscle training, and pharmacotherapy. Patients with the prevalence of a stress component of urinary incontinence receive the first-line therapy that may include surgical treatment (implantation of a transorburator suburethral sling).
In the present study, DOA diagnosis with a urodynamic test could affect the outcome of treatment, as shown in previous studies [8][12]. Bladder overactivity negatively affects subjective and objective, early and remote results after surgical treatment of urine incontinence with a middle suburethral sling [12]. Gleason et al. (2015) published that there were 64.0% versus 84.5% of successful outcomes after installing a middle suburethral sling in women with MUI and “clear” SUI, respectively. However, in women with a mixed form of urinary incontinence, there was a reduction in all symptoms and an improvement in quality of life, similar to an improvement in quality-of-life values in patients with SUI [13]. Natale et al. (2018) noted that patients with a mixed form of urinary incontinence could be recommended surgery for the stress-induced component after unsuccessful conservative therapy [14].
A small series of studies that included 42 women with MUI after surgical treatment demonstrated that a urodynamic test could provide a more precise prognosis of the outcome [15]. The authors are sure that future studies on the effectiveness of middle suburethral sling implantation in patients with a mixed form of urinary incontinence should be based on the results of urodynamic tests. The same conclusions were made by the results of the present study: patients with a mixed form of urinary incontinence should undergo urodynamic tests to establish possible prognosis of the effectiveness of surgery for the stress-induced component of urinary incontinence and reduction of DOA symptoms.
Another study showed that menopause and aged >60 years were the risk factors for a decrease in the effectiveness of middle suburethral sling implantation [14]. Similar conclusions were drawn by the authors of a Norwegian study. The authors established that women aged <60 years had fewer postoperative complications associated with urinary incontinence and women <60 years were less satisfied with the results of surgical treatment [16]. Thus, it is important to consider the risk factors for a decrease in surgery effectiveness at the stage of pre-operation counseling. The present study demonstrated that the age of the patients, excessive body weight, and initial high OABq score could be the factors that significantly worsen the prognosis of surgery.
Despite statistically significant differences in the urodynamic parameters, all of them were characterized by high variability. For example, the implantation of a suburethral sling causes clinically insignificant infra-vesical obstruction manifested as a decrease in the maximum urination rate. However, this decrease should not be considered clinically significant because there is no increase in the post-void residual volume after the surgery. The implantation of a suburethral sling did not affect maximal detrusor pressure and maximal detrusor pressure achieved at maximum urine flow.
Limitations. The present study had some limitations. A retrospective design and lack of a control group did not allow the authors to extrapolate the results to the entire general population.
Conclusion
The implementation of a synthetic suburethral sling demonstrated a significant improvement of parameters in most patients with a mixed form of urinary incontinence. The initial age >60 years, high body mass index, and initially high OABq score are the factors that worsen the prognosis of the outcome. The authors did not reveal a significant influence of surgery on DOA. Multicentral randomized studies need to be conducted to verify the obtained studies.
References
1. Minassian VA, Bazi T, Stewart WF. Clinical epidemiological insights into urinary incontinence. Int Urogynecol J. 2017;28(5):687-696. DOI: 10.1007/s00192-017-3314-7.
2. Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U, Van Kerrebroeck P, Victor A, Wein A; Standardisation Sub-Committee of the International Continence Society. The standardisation of terminology in lower urinary tract function: report from the standardisation sub-committee of the International Continence Society. Urology. 2003;61(1):37-49. DOI: 10.1016/s0090-4295(02)02243-4.
3. Dooley Y, Lowenstein L, Kenton K, FitzGerald M, Brubaker L. Mixed incontinence is more bothersome than pure incontinence subtypes. Int Urogynecol J Pelvic Floor Dysfunct. 2008;19(10):1359-62. DOI: 10.1007/s00192-008-0637-4.
4. Dmochowski R, Staskin D. Mixed incontinence: definitions, outcomes, and interventions. Curr Opin Urol. 2005;15(6):374- 9. DOI: 10.1097/01.mou.0000183946.96411.76.
5. Myers DL. Female mixed urinary incontinence: a clinical review. JAMA. 2014;311(19):2007-14. DOI: 10.1001/jama.2014.4299.
6. Kobashi KC, Albo ME, Dmochowski RR, Ginsberg DA, Goldman HB, Gomelsky A, Kraus SR, Sandhu JS, Shepler T, Treadwell JR, Vasavada S, Lemack GE. Surgical Treatment of Female Stress Urinary Incontinence: AUA/SUFU Guideline. J Urol. 2017;198(4):875-883. DOI: 10.1016/j.juro.2017.06.061.
7. Abrams P, Andersson KE, Birder L, Brubaker L, Cardozo L, Chapple C, Cottenden A, Davila W, de Ridder D, Dmochowski R, Drake M, Dubeau C, Fry C, Hanno P, Smith JH, Herschorn S, Hosker G, Kelleher C, Koelbl H, Khoury S, Madoff R, Milsom I, Moore K, Newman D, Nitti V, Norton C, Nygaard I, Payne C, Smith A, Staskin D, Tekgul S, Thuroff J, Tubaro A, Vodusek D, Wein A, Wyndaele JJ; Members of Committees; Fourth International Consultation on Incontinence. Fourth International Consultation on Incontinence Recommendations of the International Scientific Committee: Evaluation and treatment of urinary incontinence, pelvic organ prolapse, and fecal incontinence. Neurourol Urodyn. 2010;29(1):213-40. DOI: 10.1002/nau.20870.
8. Kammerer-Doak D, Rizk DE, Sorinola O, Agur W, Ismail S, Bazi T. Mixed urinary incontinence: international urogynecological association research and development committee opinion. Int Urogynecol J. 2014;25(10):1303-12. DOI: 10.1007/s00192-014-2485-8.
9. Welk B, Baverstock RJ. The management of mixed urinary incontinence in women. Can Urol Assoc J. 2017;11(6Suppl2):S121-S124. DOI: 10.5489/cuaj.4584.
10. Core Development Team R. A Language and Environment for Statistical Computing. vol. 2. Vienna, Austria: R Foundation for Statistical Computing; 2020.
11. Wu SP, Lo TS, Pue LB, Cortes EF, Lu MH, Al-Kharabsheh AM, Lin yH. Outcome after conservative management for mixed urinary incontinence. J Obstet Gynaecol Res. 2015;41(2):269-76. DOI: 10.1111/jog.12526.
12. Balachandran A, Duckett J. Does the diagnosis of detrusor overactivity affect the long-term prognosis of patients treated with a retropubic midurethral sling? Int Urogynecol J. 2016;27(12):1913-1918. DOI: 10.1007/s00192-016-3058-9.
13. Gleason JL, Parden AM, Jauk V, Ballard A, Sung V, Richter HE. Outcomes of midurethral sling procedures in women with mixed urinary incontinence. Int Urogynecol J. 2015;26(5):715-20. DOI: 10.1007/s00192-014-2580-x.
14. Natale F, Illiano E, La Penna C, Balsamo R, Costantini E. Mixed urinary incontinence: A prospective study on the effect of trans-obturator mid-urethral sling. Eur J Obstet Gynecol Reprod Biol. 2018;221:64-69. DOI: 10.1016/j.ejogrb.2017.12.003.
15. Salinas-Casado J, Méndez-Rubio S, Pesquera-Ortega L, Vírseda-Chamorro M, Gutiérrez-Martín P, Resel-Folkersma L, Esteban-Fuertes M, Moreno-Sierra J. Utilidad de la urodinámica en el tratamiento de la incontinencia urinaria femenina mixta con slings suburetrales [Usefulness of urodynamics in the treatment of mixed urinary incontinence in women with suburethral slings]. Arch Esp Urol. 2016;69(4):172-7. (In Spanish). PMID: 27225054.
16. Engen M, Svenningsen R, Schiøtz HA, Kulseng-Hanssen S. Mid-urethral slings in young, middle-aged, and older women. Neurourol Urodyn. 2018;37(8):2578-2585. DOI: 10.1002/nau.23583.
About the Authors
A. O. ZaitsevaRussian Federation
Anastasia O. Zaitseva – M.D.; Urologist; Urologist
7-9 Universitetskaya Qy, St. Petersburg, 199034
5 Stachek Sq, St. Petersburg, 198095
O. V. Volkova
Russian Federation
Olga Vladimirovna Volkova – M.D., Resident
7-9 Universitetskaya Qy, St. Petersburg, 199034
I. A. Labetov
Russian Federation
Ivan A. Labetov – Resident
7-9 Universitetskaya Qy, St. Petersburg, 199034
G. V. Kovalev
Russian Federation
Gleb V. Kovalev – M.D.; Urologist; Urologist
7-9 Universitetskaya Qy, St. Petersburg, 199034
5 Stachek Sq, St. Petersburg, 198095
D. D. Shkarupa
Russian Federation
Dmitry D. Shkarupa – M.D., Dr.Sc. (Med); Deputy CEO for Medical Care Organization; Urologist
7-9 Universitetskaya Qy, St. Petersburg, 199034
5 Stachek Sq, St. Petersburg, 198095
Review
For citations:
Zaitseva A.O., Volkova O.V., Labetov I.A., Kovalev G.V., Shkarupa D.D. Efficacy of a synthetic middle urethral sling in patients with mixed urinary incontinence. Urology Herald. 2022;10(2):53-62. (In Russ.) https://doi.org/10.21886/2308-6424-2022-10-2-53-62













































