Scroll to:
YV-plasty in the treatment of patients with recurrent bladder neck stenosis
https://doi.org/10.21886/2308-6424-2022-10-1-52-59
Abstract
Introduction. Bladder neck stenosis (BNS) is a late complication of surgical treatment for benign prostatic hyperplasia. Available methods of endoscopic correction in primary BNS have limited effectiveness, while in recurrent cases their use does not lead to satisfactory results at all. YV-plasty of the bladder neck (BN) is one of the available methods of treatment for recurrent BNS.
Purpose of the study. To evaluate the treatment results of patients with recurrent BNS using endovideoscopic YV-plasty of the BN.
Materials and methods. We retrospectively analyzed the treatment results of 8 patients with recurrent BNS who underwent endovideoscopic YV-plasty of the BN in the Urology Division No.1 of the St. Luke St. Petersburg Clinical Hospital from 2019 to 2021.
Results. Endovideoscopic YV-plasty of the bladder neck was successfully performed in all 8 patients. The mean preoperative Qmax was 3.7 ml/s (1.8 – 5.7). At 6 months after surgery, the mean Qmax was 21.4 mL/s (16.7 – 24.1). The mean preoperative I-PSS score was 20.5 (17 – 24). The mean I-PSS score 6 months after surgery was 7.1 (5.0 – 9.0). No cases of de-novo stress urinary incontinence were registered.
Conclusions. Endovideoscopic YV-plasty of the BN may be an effective and safe method of treatment of patients with recurrent BNS. However, further studies are needed to obtain long-term results.
For citations:
Popov S.V., Orlov I.N., Tsoy A.V., Topuzov T.M., Chernysheva D.Yu. YV-plasty in the treatment of patients with recurrent bladder neck stenosis. Urology Herald. 2022;10(1):52-59. (In Russ.) https://doi.org/10.21886/2308-6424-2022-10-1-52-59
Introduction
Bladder neck stenosis (BNS) is a complication develops after surgery for benign prostatic hyperplasia (BPH), which is characterized by the narrowing of the urethra at the level of the bladder neck (BN) that leads to the appearance of symptoms and signs of infra-vesical obstruction [1][2]
Statistical data on the prevalence of this pathology remain unclear. However, it is known that epidemiological indicators of this pathology have decreased in the past 20 years [3][4][5][6]. Thus, according to Bazaeva et al. (1988), the prevalence of BNS reached 24.8% [7]. In 2005, Lee et al. reported on the possibility of BNS development in 20% after surgical interventions [3]. Later, Primiceri et al. (2017) published that BNS rate did not exceed 9.6% after photoselective vaporization of the prostate, while BNS rate after bipolar transurethral prostate resection was 4.9% [5].
The tendency to a decrease in the incidence rate of BNS after the treatment of patients with BNS can be explained by a significant decrease in the number of open surgical interventions associated with significant tissue trauma [8][9]. Despite this, it should be mentioned that none of the currently available minimally invasive treatment methods is devoid of complications in the form of BNS [5].
According to available publications, the existing methods of endoscopic treatment for BNS have various efficacy [10]. Endoscopic incision and resection have a relatively satisfactory efficacy in primary BNS. However, in recurrent cases, the effectiveness of these methods is significantly reduced with each subsequent surgical intervention [11][12][13].
One of the rational methods of treatment for recurrent BNS is YV plasty of the bladder neck [14].
The study aimed to evaluate the effectiveness of YV plasty in the treatment of patients with recurrent BNS.
Materials and methods
The authors conducted a prospective analysis of the results of the treatment of eight patients with recurrent BNS, who underwent endovideoscopic YV plasty of the bladder neck at the Urology Division No. 1 of St. Luke St. Petersburg Clinical Hospital from 2019 to 2021.
In addition to the standard clinical minimum, the preoperative examination included assessment of maximum urine flow rate (Qmax), post-void residual, retrograde and voiding cystourethrography, and a blood test for prostate-specific antigen. When a reduction of the contractile function and bladder capacity was suspected, a complex urodynamic study was performed. Before and after surgical treatment, patients completed the International Prostate Symptom Score questionnaire without the assistance of a doctor.
Cystourethroscopy was used to evaluate the syntopy of anatomic structures such as the external bladder sphincter, seminal colliculus, and stenotic part of the bladder neck.
The successful outcome of the surgery was the absence of any invasive intervention (catheterization, dilation, transurethral interventions) 3 months after surgery.
Surgical technique. The patient was placed in a lithotomy position. The endovideoscopic method was used to make extraperitoneal access to the anterior bladder wall and its neck. After the mobilization of the specified anatomical structures, the second surgeon used a transurethral approach to make an incision of the stenotic BNS with the conventional 12-hours dial using a thulium laser FiberLase U2 (IPG Photonics Corp., IRE-Polus, Fryasino, Russian Federation) [power capacity – 1.5 J; frequency – 23 Hz] (Fig. 1). The specified dissection was carried out until the irrigation jet appeared in the prevesical space (Fig. 2). Therefore, the defect formed in the bladder neck was used as a reference point for a further median dissection of the stenotic area of BNS. Furthermore, the surgeon continued the specified incision in two directions at V and VII hours with the conventional 12-hour dial (Y-shaped) (Fig. 3). The triangular flap formed with the apex directed toward the prostatic urethra is sutured in the V shape (Fig. 4). The prevesical space was drained in one day. The urethral catheter was removed on Day 7 after cystography.

Figure 1. Transurethral laser incision of the bladder neck
with the conventional 12-hour dial under visual control from the prevesical space
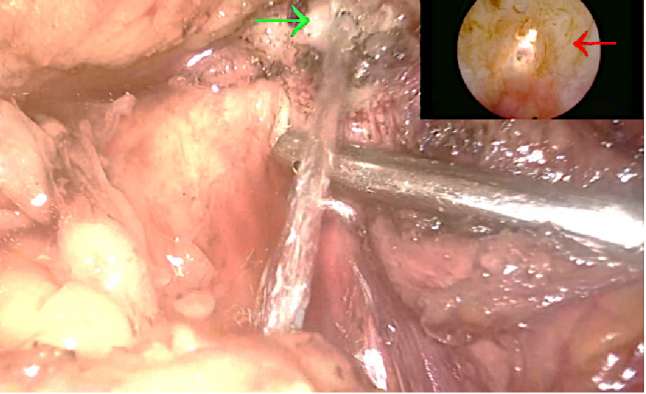
Figure 2. Appearance of a jet of irrigation fluid at the site of laser incision of the bladder neck

Figure 3. Y-shaped incision of the bladder neck and anterior bladder wall with flap formation
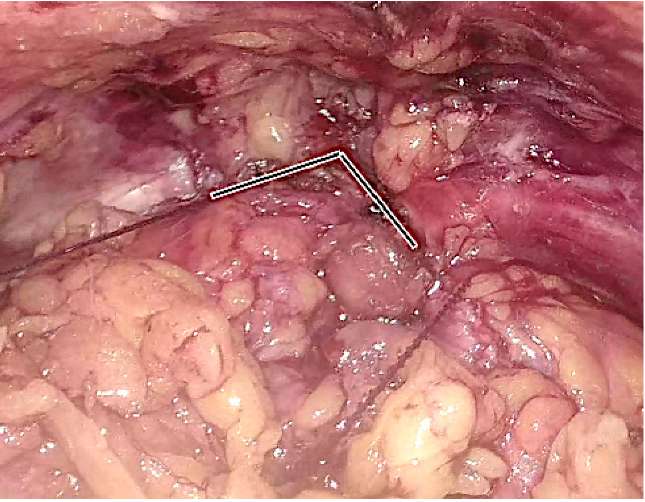
Figure 4. V-shaped suturing of the bladder neck with the anterior bladder wall
Statistical analysis. The study results were analyzed using descriptive statistical methods in IBM SPSS Statistica 25 (StatSoft Inc., IBM SPSS Corp., Tulsa, OK, USA).
Results
Eight patients underwent successful endovideoscopic YV plasty of the bladder neck. The medical history of all patients had an endoscopic intervention for BPH with further development of BNS. A typical clinical picture of this complication was a period of satisfactory micturition after endoscopic intervention with a gradual intensification of obstruction symptoms. The time to development of BNS after BPH was 11–14 weeks. The time to recurrence varied from 3 to 8 weeks. The average age of the operated patients was 68 (58–72) years. Seven out of eight patients had two and more endoscopic interventions for BNS in their medical history. A patient had this type of intervention performed immediately after the first recurrence. The mean volume of blood loss was 82 (50–150) ml. The mean time of surgery was 82 (57–121) minutes. Six months after the surgery, obstructive symptoms resolved in all patients (mean Qmax – 21.4 ml/s). In one patient, 14 months later, a decrease in Qmax was recorded at 12.1 ml/s without a significant increase in post-void residual volume (25 ml). There were no de novo cases of stress urinary incontinence. The severity of complications in all cases was limited by degree I (Clavien-Dindo scale). The total scores are presented in Table 1.
Table 1. Patients’ demographics
|
Demographics |
Indicator |
|
Number of patients, n |
8 |
|
Average age, years (min – max) |
68 (58–72) |
|
Endoscopic procedures, n (min – max) |
2.3 (1.0–4.0) |
|
Average blood loss, ml (min – max) |
82 (50–150) |
|
Follow-up period, months (min – max) |
13.6 (7.0–20.0) |
|
Mean preoperative Q max, ml/sec (min – max) |
3.7 (1.8–5.7) |
|
Mean Q max after 6 months, ml/sec (min – max) |
21.4 (16.7–24.1) |
|
Mean preoperative PVR urine, ml/sec (min – max) |
143 (95–210) |
|
Mean PVR urine after 6 months, ml/sec (min – max) |
14 (0–30) |
|
Average IPSS before surgery, pts (min – max) |
20.5 (17.0–24.0) |
|
Average IPSS after 6 months, pts (min – max) |
7.1 (5.0–9.0) |
|
Average QoL before surgery, pts (min – max) |
5 (4–6) |
|
Average QoL after 6 months, pts (min – max) |
2 (1–3) |
Note: Qmax – maximum urine flow rate; PVR – post-void residual;
IPSS – International Prostate Symptom Score; QoL – Quality of Life associated with urination
Discussion
Currently, the treatment of recurrent BNS remains an unsolved issue in modern urology. The effectiveness of dilation, incision, and resection of BNS decreases with each subsequent intervention [15]. Often, a short recurrence-free period leads to the need for permanent urine diversion [16].
The low effectiveness of endoscopic methods makes researchers search for alternative solutions. In 1953, Young proposed an original method of YV plasty for patients with BNS [17]. The approach is based on the formation of a well-vascularized flap of the anterior bladder wall for the augmentation of the stenotic bladder neck. Despite the simplicity of the proposed method, it became widespread only after the development of robot-assisted surgery, which allows accurate manipulation around the bladder neck.
In our research centre, this approach was realized using an endovideoscopic approach with the modification for transurethral access. The application of transurethral laser dissection of the stenotic area significantly facilitates the precise dissection of the bladder neck, which reduces the damage of the surrounding tissues. The latter plays a key role in the development of cicatricle processes.
The major drawbacks of this study include a small sampling in the studied group and a limited follow-up period. Furthermore, the absence of recurrence in patients was confirmed only by non-invasive methods; the control cystourethroscopy was not performed.
Conclusion
The proposed modification of the endovideoscopic YV plasty of the bladder neck may be an effective and safe treatment method for patients with recurrent BNS that developed after BPH. This treatment method is not associated with significant high intraoperative and postoperative complications. However, a longer follow-up period is required to obtain remote results.
References
1. Latini JM, McAninch JW, Brandes SB, Chung JY, Rosenstein D. SIU/ICUD Consultation On Urethral Strictures: Epidemiology, etiology, anatomy, and nomenclature of urethral stenoses, strictures, and pelvic fracture urethral disruption injuries. Urology. 2014;83(3 Suppl):S1-7. DOI: 10.1016/j.urology.2013.09.009.
2. Popov S.V., Orlov I.N., Tsoy A.V., Chernysheva D.Yu. Bladder neck stenosis after surgical treatment of patients with benign prostatic hyperplasia. Epidemiology. Modern treatment options. Experimental and Clinical Urology. 2021;14(1):100-107. DOI: 10.29188/2222-8543-2021-14-1-100-107.
3. Lee YH, Chiu AW, Huang JK. Comprehensive study of bladder neck contracture after transurethral resection of prostate. Urology. 2005;65(3):498-503; discussion 503. DOI: 10.1016/j.urology.2004.10.082.
4. Grechenkov A, Sukhanov R, Bezrukov E, Butnaru D, Barbagli G, Vasyutin I, Tivtikyan A, Rapoport L, Alyaev Y, Glybochko P. Risk factors for urethral stricture and/or bladder neck contracture after monopolar transurethral resection of the prostate for benign prostatic hyperplasia. Urologia. 2018;85(4):150-157. DOI: 10.1177/0391560318758195.
5. Primiceri G, Castellan P, Marchioni M, Schips L, Cindolo L. Bladder Neck Contracture After Endoscopic Surgery for Benign Prostatic Obstruction: Incidence, Treatment, and Outcomes. Curr Urol Rep. 2017;18(10):79. DOI: 10.1007/s11934-017-0723-6.
6. Talat M, Abdrabuh AM, Elhelali M, Elsotohi I, Eleweedy S. Safety and efficacy of transurethral vaporization of the prostate using plasma kinetic energy: Long-term outcome. Urol Ann. 2019;11(2):175-179. DOI: 10.4103/UA.UA_76_18.
7. Bazaev B.B., Trapeznikova M.F. MAP. Otdalennye oslozhnenija adenomjektomii prostaty. 1988. (In Russ.).
8. Kaynar M, Gul M, Kucur M, Çelik E, Bugday MS, Goktas S. Necessity of routine histopathological evaluation subsequent to bladder neck contracture resection. Cent European J Urol. 2016;69(4):353-357. DOI: 10.5173/ceju.2016.874.
9. Kidd EA, Stewart F, Kassis NC, Hom E, Omar MI. Urethral (indwelling or intermittent) or suprapubic routes for short-term catheterisation in hospitalised adults. Cochrane Database Syst Rev. 2015;2015(12):CD004203. DOI: 10.1002/14651858.CD004203.pub3.
10. Ramirez D, Simhan J, Hudak SJ, Morey AF. Standardized approach for the treatment of refractory bladder neck contractures. Urol Clin North Am. 2013;40(3):371-80. DOI: 10.1016/j.ucl.2013.04.012.
11. Simhan J, Ramirez D, Hudak SJ, Morey AF. Bladder neck contracture. Transl Androl Urol. 2014;3(2):214-20. DOI: 10.3978/j.issn.2223-4683.2014.04.09.
12. Redshaw JD, Broghammer JA, Smith TG 3rd, Voelzke BB, Erickson BA, McClung CD, Elliott SP, Alsikafi NF, Presson AP, Aberger ME, Craig JR, Brant WO, Myers JB. Intralesional injection of mitomycin C at transurethral incision of bladder neck contracture may offer limited benefit: TURNS Study Group. J Urol. 2015;193(2):587-92. DOI: 10.1016/j.juro.2014.08.104.
13. Furr J, Gelman J. Endoscopic Management of Urethral Stricture Disease and Bladder Neck Contractures. J Endourol. 2020;34(S1):S7-S12. DOI: 10.1089/end.2018.0317.
14. Musch M, Hohenhorst JL, Vogel A, Loewen H, Krege S, Kroepfl D. Robot-assisted laparoscopic Y-V plasty in 12 patients with refractory bladder neck contracture. J Robot Surg. 2018;12(1):139-145. DOI: 10.1007/s11701-017-0708-y.
15. Pansadoro V, Emiliozzi P. Iatrogenic prostatic urethral strictures: classification and endoscopic treatment. Urology. 1999;53(4):784-9. DOI: 10.1016/s0090-4295(98)00620-7.
16. Spahn M, Kocot A, Loeser A, Kneitz B, Riedmiller H. Last resort in devastated bladder outlet: bladder neck closure and continent vesicostomy--long-term results and comparison of different techniques. Urology. 2010;75(5):1185-92. DOI: 10.1016/j.urology.2009.11.070.
17. Young BW. The retropubic approach to vesical neck obstruction in children. Surg Gynecol Obstet. 1953;96(2):150-4. PMID: 13015363.
About the Authors
S. V. PopovRussian Federation
Sergey V. Popov — M.D., Dr.Sc. (Med), Full Prof.; Prof.
Chief Medical Officer
St. Petersburg
I. N. Orlov
Russian Federation
Igor N. Orlov — M.D., Cand.Sc.(Med); Head, Urology Division No.1, City Centre of Endoscopic Urology and New Technologies
Dept. of Urology
St. Petersburg
A. V. Tsoy
Russian Federation
Alexey V. Tsoy — M.D.; Urologist, Urology Division No.1, City Centre of Endoscopic Urology and New Technologies
St. Petersburg
T. M. Topuzov
Russian Federation
Timur M. Topuzov — M.D., Cand.Sc. (Med); Urologist, Urology Division No.1, City Centre of Endoscopic Urology and New Technologies
St. Petersburg
D. Yu. Chernysheva
Russian Federation
Daria Yu. Chernysheva - M.D., Cand.Sc. (Med); Urologist, Urology Division No.1, City Centre of Endoscopic Urology and New Technologies
Assist., Dept. of Advanced Surgery, Medical Faculty
St. Petersburg
Review
For citations:
Popov S.V., Orlov I.N., Tsoy A.V., Topuzov T.M., Chernysheva D.Yu. YV-plasty in the treatment of patients with recurrent bladder neck stenosis. Urology Herald. 2022;10(1):52-59. (In Russ.) https://doi.org/10.21886/2308-6424-2022-10-1-52-59













































