Scroll to:
Percutaneous antegrade ureterolithotripsy for proximal ureteral stones: overview own experience use
https://doi.org/10.21886/2308-6424-2021-9-2-92-99
Abstract
Introduction. Currently, a large number of techniques are used in the treatment of patients with ureteral stones: extracorporeal shock-wave lithotripsy (ESWL), retrograde ureterolithotripsy (RULT), laparoscopic and retro-peritoneoscopic ureterolithotomy.
Purpose of the study. To evaluate the possibilities and effectiveness of percutaneous antegrade ureterolithotripsy in the treatment of patients with proximal ureteral stones in comparison with transurethral contact ureterolithotripsy.
Materials and methods. Twenty-eight patients with urolithiasis were treated, who underwent percutaneous antegrade ureterolithotripsy (PAULT) and 27 patients of the control group, who underwent RULT. All patients included in the study underwent a standard preoperative examination: complete blood count and urine analysis, bacteriological urine culture, biochemical tests, and X-ray research methods. Plain urography, renal ultrasound, computed tomography were used as imaging methods. The OLYMPUS URF-V3 8.4 Ch (Olympus Europa SE & Co. KG., Germany) video uretero-renoscope was used for PAULT in patients of the main group; lithotripsy was performed using thulium laser. The results of the study were subjected to statistical processing in order to determine the statistical significance of the differences between the data obtained. Quantitative variables were described using the arithmetic mean (M) and standard deviation (5). Qualitative variables were estimated by absolute and relative frequencies (percentages). The data were considered reliable at p values < 0.05.
Results. The average time of surgical intervention in patients of the main group from the moment of placement of the ureteral catheter was 47 ± 12 min, with access without preliminary renal catheterization: 28 ± 4 min. Average time of surgical intervention in patients of the control group: 42.0 ± 10.7 minutes. The presented data indicate a significant (p < 0.05) greater cases' number of complete stone removal among patients of the main group compared with patients in the control group (74.0%).
Conclusion. PAULT is preferred among choice treatment methods for patients with proximal ureteral large stones, for whom RULT and ESWL cannot be performed with a high level of “stone-free” rate and a minimum number of complications.
Keywords
For citations:
Popov S.V., Guseinov R.G., Gadjiev N.K., Davydov A.V., Obidnyak V.M., Barhitdinov R.S., Perepelitsa V.V. Percutaneous antegrade ureterolithotripsy for proximal ureteral stones: overview own experience use. Urology Herald. 2021;9(2):92-99. (In Russ.) https://doi.org/10.21886/2308-6424-2021-9-2-92-99
Introduction
The issue of urinary stone disease (USD) remains acute worldwide because of a continuous increase in the morbidity rate, which is 0.5–5.3% annually [1][2]. In the Russian Federation, the rate of patients with USD increased by 17.3% during the past decade [3]. In 70% of patients, USD is diagnosed at the age of 30–60 years old, primarily, in men [4][5]. The issue of the method of choice for USD surgery remains open [6][7][8][9][10]. There are presently a lot of methods for the treatment of patients with ureter stones that include extracorporeal shock-wave lithotripsy (ESWL), retrograde ureterolithotripsy (RULT), laparoscopic, and retro-peritoneoscopic ureterolithotomy [11].
During the past decade, RULT was acknowledged as a low-invasive method of treatment for ureter stones [11]. The development of new endoscopic tools (small-diameter ureteroscopes, flexible ureteral nephroscopes) and laser technologies made RULT the method of choice for the treatment of ureteral stones. The application of these equipment leads to a reduction of the treatment period, a decrease in the rate of intra- and postoperative complications, and an increase in economic efficiency [12][13].
RULT is an effective method of treatment for urolithiasis of the mid and lower third of the ureter. However, in some cases (anatomic-physiological peculiarities of the ureter or strictures that complicate the access to the proximal section), RULT cannot be performed effectively. Besides, stones >1 cm that were present in the ureteral lumen for a long time (impacted stones) lead to alterations in the ureter walls and can increase the rate of complications [14]. The advantages of antegrade fragmentation include the possibility of application of larger tools, wide lumen of the ureter above the stone, better visualization of the ureter during the access, a low risk of distal migration of fragments in patients with impacted stones, and the possibility of fragment extraction without the risk of damage and ureter detachment [15].
When ESWL is not feasible (ureter stricture, high density of stones, ineffective previous treatment) and the application of RULT is contraindicated or can lead to complications, an alternative endoscopic method of treatment is percutaneous antegrade ureterolithotripsy (PAULT) [16].
The study aimed to evaluate the effectiveness of percutaneous antegrade ureterolithotripsy in the treatment of patients with proximal ureteral stones in comparison with contact ureterolithotripsy.
Materials and Methods
A total of 55 patients with proximal ureteral stones were studied. The authors analyzed the results of the treatment of 28 patients that underwent PAULT (main group) and 27 patients from the control group that underwent RULT (Table 1).
Both groups were homologous by the age and sex of the participants. The mean size of stones in the main and control groups was 12 ± 1.2 mm and 14 ± 1.3 mm, respectively. There were no statistically significant differences in the localization and density of stones in the groups (Tables 1 – 3).
Table 1. Patients’ demographics
|
Patients’ demographics |
Main group |
Control group |
||
|
Abs. |
% |
Abs. |
% |
|
|
Women |
17 |
60.7 |
15 |
55.6 |
|
Men |
11 |
39.3 |
12 |
44.4 |
|
Total |
28 |
100 |
27 |
100 |
|
Average age, years |
51.0 ± 2.55 |
52.0 ± 2.6 |
||
Table 2. Stone density
|
Stone density |
Main group |
Control group |
||
|
Abs. |
% |
Abs. |
% |
|
|
Density < 800 (HU) |
9 |
32.1 |
7 |
25.9 |
|
Density 801–1000 (HU) |
14 |
50.0 |
12 |
44.5 |
|
Density > 1001 (HU) |
5 |
17.9 |
8 |
29.6 |
Table 3. Side and localization of ureteral stones
|
Method of treatment |
Side |
Localization |
||||||
|
Right |
Left |
Upper third |
Middle third |
|||||
|
n |
% |
n |
% |
n |
% |
n |
% |
|
|
PAULT |
15 |
53.6 |
13 |
46.4 |
17 |
60.7 |
11 |
39.3 |
|
RULT |
13 |
48.1 |
14 |
51.9 |
17 |
63 |
10 |
37 |
|
Notes: PAULT – percutaneous antegrade ureterolithotripsy; RULT – retrograde ureterolithotripsy |
||||||||
Criteria of inclusion: stone > 10 mm, localization above the crossing of ureters with iliac vessels, hydronephrosis. Criteria of exclusion: pregnancy, application of anticoagulants, exacerbation of the urinary tract infection.
All patients included in the study underwent a standard preoperative examination: complete blood count and urine analysis, bacteriological urine culture, biochemical tests, and computed tomography (CT).
RULT was performed with a semi-rigid ureteroscope OLYMPUS Wa29048a. PAULT was performed with a video uretero-renoscope OLYMPUS URF-P5. Lithotripsy was made with a thulium laser and 200 µm fibers. The surgeons applied fragmentation and disintegration modes. Before the surgery, the stone size was calculated by the measurement of its largest diameter. The time of surgery was registered from the ureteral catheterization to the end of renal cavity system drainage. When the access was provided without preliminary catheterization, the time was registered from the puncture of the cavity system. The criteria of effectiveness of surgery were complete removal of stones or presence of residual concrements ≤ 3 mm. The control of residual stones was performed with flexible ureteronephroscopy at the end of surgery and CT that was conducted 24 hours after the surgery.
Surgical technique. Surgical interventions were performed under endotracheal anaesthesia because this type of anaesthesia is more preferable in cases of kidney puncture and a safe option for ureteronephrolithotripsy (possibility to use apnoe). Antegrade ureterolithotripsy was performed in the supine Valdivia-Galdakao position of a patient. The first stage was performed in a lithotomy position of a patient. Under X-ray control, ureteral catheterization with a 6–7 Ch catheter was made through transurethral access. If it was impossible to introduce a guidewire above the stone, the ureteral catheter was left distal to the stone. After that, a urethral catheter 16 Ch was introduced and ligated to the ureteral catheter. The second stage of surgery was controlled by ultrasonic and X-ray equipment and included percutaneous puncture of the pyelocalyceal system (PCS). After antegrade contrasting of the PCS, a guidewire was introduced in the needle lumen. Further, one-step bougienage of the puncture to 14 Ch was made and ureteral access sheath 12–14 Ch was installed. The surgeons preferred to introduce the guidewire into the ureter, which provided the sheath access directly to the stone. This manipulation improved the visualization of the stone due to good irrigation, reduced the time of surgery, and preserved the operational life of the flexible ureteronephroscope. Percutaneous puncture had the following criteria of access for PAULT: obtuse angle between the calyx axis that was punctured and the axis of the ureter’s upper third; maximally short access; and puncture through the calyx that contained a stone (if any). In some cases (expressed hydronephrosis, nephrostomy drainage), PAULT started with a PCS puncture and/or antegrade ureterolithotripsy. After the visualization and fragmentation of the stone with laser, fragments were removed with lithoextractors and irrigation fluid. After the stone removal, control ureteronephroscopy was performed that helped to decide on the necessity of antegrade drainage of PCS. RULT was conducted according to a standard method in the lithotomy position under endotracheal anaesthesia. After urethrocystoscopy, a hydrophilic guidewire was introduced in the ureter orifice on the respective side under X-ray control. Further, a ureteroscopy was performed. After visualization of the stone and its fragmentation with laser exposure, the fragments were removed with lithoextractors. Control ureteroscopy was performed to decide on the necessity of retrograde draining of the PCS.
In the postoperative period, a visual-analogue pain scale was used to evaluate the intensity of postoperative pain syndrome, as well as the required doses of pain-relieving drugs. Postoperative complications were defined by the Clavien-Dindo classification.
Statistical analysis. Statistical processing of the obtained data was performed using Microsoft Excel 2007 and the software package Statistica 8.0 for Windows (StatSoft Inc., USA). Quantitative variables were described using the arithmetical mean (M) and standard deviation (δ). Qualitative variables were estimated by absolute and relative frequencies (percentages). The data were significant at p < 0.05.
Results
The average time of surgical intervention in patients of the main group from the moment of placement of the ureteral catheter was 47 ± 12 min. The surgeries without preliminary renal catheterization lasted for 28 ± 4 min. The average time of surgical intervention in patients of the control group was 42.0 ± 10.7 minutes.
A comparative characteristic of the degree of stone extraction in patients after PAULT and RULT is presented in Fig. 1.
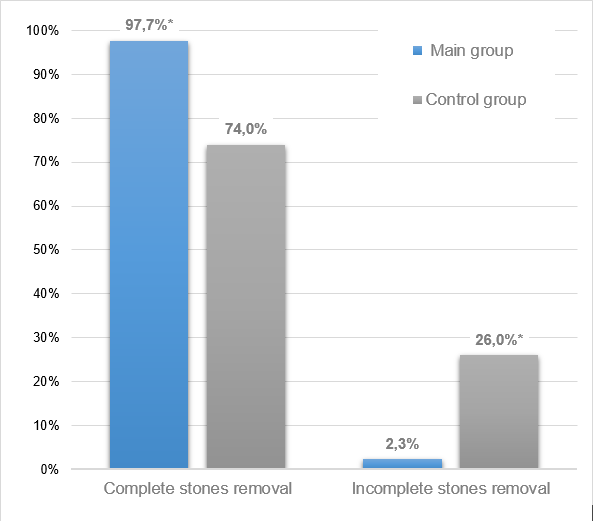
Fig. 1. Comparative characteristics of the stone removal stage in patients from the main and control groups (in percentage)
The presented data indicate a significant rate (p < 0.004) of stone-free status among patients from the main group in comparison with patients from the control group (74.0%).
Nineteen patients from the control group that underwent RULT had a ureteral stent installed, 8 patients had a ureteral catheter installed. The ureter catheter was removed on Day 1 after the surgery. Twenty-four patients (85.7%) from the main group had PAULT as a monotherapy. Four patients (14.3%) had simultaneous nephrolithotripsy. Totally tubeless surgery was performed on 20 patients. Eight patients had antegrade ureter stent placed. The removal of the ureter stent was performed 14–28 days after PAULT. In 26% of patients from the control group, residual stones > 3 mm in diameter were revealed that required ESLW or repeated ureteropyeloscopy.
The mean number of postoperative inpatient days among patients from the main group was 4 ± 1.3; the control group – 5.4 ± 2.2 days.
Postoperative complications of I–II degrees (Clavien-Dindo classification) were revealed in 4 (14.3%) patients from the main group and 3 patients (11.1%) from the control group. There were no hemorrhagic complications revealed that required hemotransfusion among the patients from the main and control groups.
Discussion
The main aim of the treatment for upper third ureteral stones is a complete extraction of stones for the removal of obstruction, prevention of further stone growth, normalization of urine passage, resolution of pain syndrome, and prevention of inflammatory complications [17]. According to the published data, percutaneous and retrograde ureterolithotripsy are feasible and effective methods of treatment for large upper third ureteral stones. The criteria for PAULT included the size of stone > 10 mm, localization of the stone above the crossing of the ureters with iliac vessels, hydronephrosis, presence of stones in the ipsilateral kidney, and anatomic peculiarities that complicate retrograde access (ureter stricture, pathologies that complicate lithotomy position of the patient, a history of surgery involving the bladder or ureter). Other factors that should be accounted for when deciding on PAULT include the time of presence of stones in the ureter, thickness of the ureter wall (measured by CT) in the location of the stone, and lack of contrasting of the ureter distal to the stone during CT [18][19]. The results of the study showed that one of the main advantages of PAULT or upper third ureteral stones was better endoscopic visualization. Besides, instrumental backup of the surgery significantly exceeds the possibilities of any transurethral ureteroscopy. The advantages of antegrade fragmentation of stones include reliable access to a kidney, usage of larger size tools, a wide lumen of the ureter above the stone, a low risk of distal migration of fragments in patients with impacted stones, and the possibility to extract the stone fragments without the risk of ureter damage or detachment.
Conclusion
Percutaneous antegrade ureterolithotripsy is a preferable method of choice in the treatment for patients with large proximal ureteral stones that cannot be extracted using contact or extracorporeal ureterolithotripsy that is characterized by a high rate of stone-free status and minimal rate of complications.
References
1. Dwyer ME, Krambeck AE, Bergstralh EJ, Milliner DS, Lieske JC, Rule AD. Temporal trends in incidence of kidney stones among children: a 25-year population based study. J Urol. 2012;188(1):247-52. DOI: 10.1016/j.juro.2012.03.021
2. Marickar YM, Vijay A. Female stone disease: the changing trend. Urol Res. 2009;37(6):337-40. DOI: 10.1007/s00240-009-0216-2
3. Apolikhin O.I., Sivkov A.V., Beshliev D.A., Solntseva T.V., Komarova V.A. Analysis of urological morbidity in the Russian Federation according to official statistics. Experimental and clinical urology. 2010;(1):4-10. (In Russ.). eLIBRARY ID: 17418791
4. Apolikhin O.I., Kakorina E.P., Sivkov A.V., Beshliev D.A., Solntseva T.V., Komarova V.A. Official statistics on urological morbidity in the Russian Federation. Urologiia. 2008;(3):3-9. (In Russ.). eLIBRARY ID: 11520901
5. Bartoletti R, Cai T, Mondaini N, Melone F, Travaglini F, Carini M, Rizzo M. Epidemiology and risk factors in urolithiasis. Urol Int. 2007;79 Suppl 1:3-7. DOI: 10.1159/000104434
6. Popov S.V., Novikov A.I., Gorgotsky I.A., Orlov I.N., Chernyshova D.Yu. Place of transurethral contact nephroli-thotripsy in the treatment of patients with kidney stones. Urologiia. 2012;(5):81-85 (In Russ.). PMID: 23342622
7. Skolarikos A. Medical treatment of urinary stones. Curr Opin Urol. 2018;28(5):403-407. DOI: 10.1097/MOU.0000000000000523
8. Komiakov B.K., Guliev B.G., Alekseev M.Iu., Shibliev R.G. Percutaneous surgery of diseases of the kidneys and urinary tracts. Vestn Khir Im I I Grek. 2011;170(4):99-101. PMID: 22191269
9. Bell TV. Unenhanced helical CT criteria to differentiate distal ureteral calculi from pelvic phleboliths. Radiology. 2007;(5): 363-367. DOI: 10.1148/radiology.207.2.9577482
10. Seitz C. Secondary signs of non-enhanced CT prior to laser ureterolithotripsy: is treatment outcome predictable? J Endourol. 2008;22(3):415-8. DOI: 10.1089/end.2007.0248
11. Turk C, Petrik A, Sarica K, Seitz C, Skolarikos A, Straub M, Knoll T. EAU Guidelines on Interventional Treatment for Urolithiasis. European Urology. 2016;69(3):475-82. DOI: 10.1016/j.eururo.2015.07.041
12. Gupta PK. Is the holmium:YAG laser the best intracorporeal lithotripter for the ureter? A 3-year retrospective study. J Endourol. 2007;21(3):305-9. DOI: 10.1089/end.2006.0247
13. Wolf JS. Treatment selection and outcomes: ureteral calculi. Urol. Clin. North Am. 2007;34(3):421-30. DOI: 10.1016/j.ucl.2007.04.010
14. Rosette J, Denstedt J, Geavlete P. The clinical research office of the endourological society ureteroscopy global study: indications, complications and outcomes in 11,885 patients J. Endourol. 2014;28(2):131-9. DOI: 10.1089/end.2013.0436
15. Wang Y, Zhong B, Yang X, Wang G, Hou P, Meng J. Comparison of the efficacy and safety of URSL, RPLU, and MPCNL for treatment of large upper impacted ureteral stones: a randomized controlled trial. BMC Urol. 2017;17(1):50 DOI: 10.1186/s12894-017-0236-0
16. Winter M, Lynch C, Appu S, Kourambas J. Access shealth-aided percutaneous antegrade ureteroscopy; a novel approach to the ureter. BJU Int. 2011 Aug;108(4):620-2. DOI: 10.1111/j.1464-410X.2011.10538.x
17. Gu XJ, Lu JL, Xu Y. Treatment of large impacted proximal ureteral stones: randomized comparison of minimally invasive percutaneous antegrade ureterolithotripsy versus retrograde ureterolithotripsy. World J Urol. 2013;31:1605-1610. DOI: 10.1089/end.2007.0230
18. Drake T, Grivas N, Dabestani S, Knoll T, Lam T, Maclennan S, Petrik A, Skolarikos A, Straub M, Tuerk C, Yuan CY, Sarica K. What are the Benefits and Harms of Ureteroscopy Compared with Shock-wave Lithotripsy in the Treatment of Upper Ureteral Stones? A Systematic Review. Eur Urol. 2017;72(5):772-786. DOI: 10.1016/j.eururo.2017.04.016
19. Ohen J, Cohen S, Grasso M. Ureteropyeloscopic treatment of large, complex intrarenal and proximal ureteral calculi. BJU Int. 2013;111:E127. DOI: 10.1111/j.1464-410X.2012.11352.x 5
About the Authors
S. V. PopovRussian Federation
Sergey V. Popov — M.D., Dr.Sc. (M), Full Prof.; Prof., Dept. of Urology, S.M. Kirov Military Medical Academy; Chief Medical Officer, St. Luke Clinical Hospital.
194044, St. Petersburg, 46 Chugunnaya st.; 194044, St. Petersburg, 37A Academician Lebedev st.
Competing Interests:
The authors declare no conflicts of interest.
R. G. Guseinov
Russian Federation
Ruslan G. Guseynov — M.D.; Head, Urology Division No. 2, St. Luke Clinical Hospital.
194044, St. Petersburg, 46 Chugunnaya st.
Tel.: +7 (931) 229-29-53
Competing Interests:
The authors declare no conflicts of interest.
N. K. Gadjiev
Russian Federation
Nariman K. Gadjiev — M.D., Dr.Sc.(M); Head, ESWL and Endovideosurgery Division, Research Center of Urology, Pavlov First St. Petersburg State Medical University.
197022, St. Petersburg, 6-8 Lev Tolstoy st.
Competing Interests:
The authors declare no conflicts of interest.
A. V. Davydov
Russian Federation
Aleksey V Davydov — M.D., Cand.Sc.(M); Urologist, Urology Division No. 2, St. Luke Clinical Hospital.
194044, St. Petersburg, 46 Chugunnaya st.
Competing Interests:
The authors declare no conflicts of interest.
V. M. Obidnyak
Russian Federation
Vladimir M. Obidnyak — M.D.; Urologist, ESWL and Endovideosurgery Division, Research Center of Urology, Pavlov First St. Petersburg State Medical University.
197022, St. Petersburg, 6-8 Lev Tolstoy st.
Competing Interests:
The authors declare no conflicts of interest.
R. S. Barhitdinov
Russian Federation
Rinat S. Barchitdinov — M.D.; Urologist, Urology Division No. 2, St. Luke Clinical Hospital.
194044, St. Petersburg, 46 Chugunnaya st.
Competing Interests:
The authors declare no conflicts of interest.
V. V. Perepelitsa
Russian Federation
Vitaliy V. Perepelitsa — M.D., Cand.Sc.(M); Urologist, Urology Division No. 2, St. Luke Clinical Hospital.
194044, St. Petersburg, 46 Chugunnaya st.
Competing Interests:
The authors declare no conflicts of interest.
Review
For citations:
Popov S.V., Guseinov R.G., Gadjiev N.K., Davydov A.V., Obidnyak V.M., Barhitdinov R.S., Perepelitsa V.V. Percutaneous antegrade ureterolithotripsy for proximal ureteral stones: overview own experience use. Urology Herald. 2021;9(2):92-99. (In Russ.) https://doi.org/10.21886/2308-6424-2021-9-2-92-99













































