Scroll to:
Advancement urethroplasty for distal hypospadias repair without dismembering urethra spongy body and glans penis
https://doi.org/10.21886/2308-6424-2020-8-3-5-12
Abstract
Introduction. Hypospadias is one of the most common urological pathology in boys requiring surgical correction. Currently, the literature describes more than 300 different techniques for correcting hypospadias. This indicates a lack of ideal methods and standards of treatment that satisfy most pediatric surgeons and urologists. The distension methods of treatment for hypospadias have not been extremely demand in recent decades. The relatively high frequency of the meatostenosis formation in the postoperative period is one of the factors limiting the spread of the method. We suppose that the development of modifications of the surgical technique for relocating urethroplasty aimed at reducing the incidence of postoperative meatostenosis is an urgent area.
Purpose of the study. To evaluate the experience of using advancement urethroplasty in the treatment of hypospadias distal forms.
Materials and methods. We present a modified method for correction of hypospadias distal forms — advancement urethroplasty without dismembering urethral spongy body and glans penis. The proposed method allows you to form a meatus in a physiological position without a urethral suture, with the restoration of the integrity of the spongy body, without it cutting off during mobilization in the distal section. The standard C.A. Beck technique was used for treatment in 44 patients — group I. According to the author's method, 60 boys were operated on in the period from 2016 to 2018 — group II. Postoperative follow-up period lasted 6 - 36 months. All patients were evaluated in terms of cosmetic results and the incidence of postoperative complications.
Results. The high efficiency of the proposed urethroplasty technique was shown. There was a decrease in the number of postoperative complications compared to the classical method of advancement urethroplasty. Reoperations were required in 5% of cases. The cosmetic results obtained after moving urethroplasty in both groups were identical and were assessed by parents and the operating surgeon as excellent.
Conclusions. It is advisable to use moving urethroplasty in case of distal hypospadias with not prolonged urethral dysplasia proximal to the meatus and diastasis between the meatus and its physiological position not exceeding 1 cm. Relocating urethroplasty with non-dissecting spongioplasty provides a lower incidence of meatostenosis in the postoperative period compared to the classical Beck teсhnique.
For citations:
Akramov N.R., Kagantsov I.M., Sizonov V.V., Batrutdinov R.T., Dubrov V.I., Khaertdinov E.I. Advancement urethroplasty for distal hypospadias repair without dismembering urethra spongy body and glans penis. Urology Herald. 2020;8(3):5-12. https://doi.org/10.21886/2308-6424-2020-8-3-5-12
Introduction
Hypospadias is one of the frequent urological pathologies in boys requiring surgical correction and is found according to modern literature in 1:125 - 1:300 newborn boys [1][2][3]. The distal forms (glandular, subcoronal and distal penile) account for 65 - 70% of all forms of hypospadias [4].
At the present day, there are more than 300 known methods of surgical management of hypospadias [5][6], but the using of these corrective surgeries does not preclude from the formation of urethral fistula, urethra disruption and meatal stenosis, which determines the continuation of the optimal method of correction searching.
The first to propose the distension technique of urethroplasty without the neourethra formation was C.A. Beck in 1898 [7]. The essence of the technique was to separate the distal part of the urethra from the cavernosum, mobilize the edges of the glans penis, advance the urethra without tension to its physiological rest position and suture the glans tissues over it. Later in 1931, 5.A. Koff modified the technique and used it in 21 patients with an excellent result, which gave the technique a new popularizing impulse [8]. At the present day, distension techniques have not found widespread clinical use, as confirmed by single reports of advancement urethroplasty use in the modern literature [9][10][11][12][13].
Materials and methods
In all patients, the pathology was revealed in the course of preventive examination of children or during outpatient visiting of a pediatric surgeon, paediatrician, pediatric urologist-andrologist, and pediatric endocrinologist.
Study design: an open, multicentral, simple, case-controlled, prospective clinical study.
Patients eligibility criterion for the relocating urethroplasty was distal hypospadias, in which the diastasis between the meatus and the physiological location of the external urethral opening was no more than 1 cm, together with the absence of penile curvature.
All patients were divided into two groups: Group I - a comparison group comprising 44 boys operated according to advancement urethroplasty technique in Beck C.A. modification within the period from 2015 till 2018. Among them were 6 (13.6%) glandular, 19 (43.2%) subcoronal, and 19 (43.2%) distal penile forms. The average age of boys was 49.8 months.
Group II is a study group, which included 60 patients operated according to proposed by us advancement urethroplasty with nondismembering spongioplasty within the period from 2016 till 2018 [14]. Among them were 7 (11.7%) glandular, 31 (51.7%) subcoronal, and 22 (36.6%) distal penile forms. The average age of boys was 46.8 months.
The classical technique of advancement urethroplasty was performed as follows. An incision was made around the meatus, it was extended in the line of the midline along the glans penis, down the median raphe along the ventral surface, and a circumferential incision of skin below the coronal sulcus. The distal section of the urethra was separated from the cavernous bodies together with the meatus. The mobilized urethra was moved upward and laid without tension between the edges of the glans penis. The external urethral opening was formed in the physiological rest position by fixing the edges of the mobilized urethra to glans penis with interrupted atraumatic sutures. The glans penis was hurled together over the advanced distal urethra. The postoperative wound was sutured using nodular atraumatic sutures. a urethral catheter was placed in the urinary bladder and a circular compression bandage was applied around the penis.
The modified technique of advancement urethroplasty with non-dismembering spongioplasty was carried out as follows. The boundaries of subsequent sections were marked (Fig. 1).
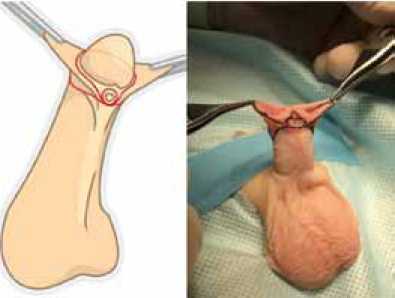
Figure 1. Marking cut lines
Рисунок 1. Разметка линий разрезов
A circumferential incision of skin was made more proximal of coronal sulcus on 4 - 6 mm and an edging incision around the external urethral opening with 1 - 2 mm penile skin. The penile skin was mobilized up to its base. Excision of the strands was carried out in the presence of curvature of the penis. Urethra with the spongious body was separated from the cavernous bodies depending on the diastasis of misplaced meatus of the urethra and its physiological position throughout 20 - 50 mm without cutting off the bifurcated distal segment of the spongious body from the glandular part of the urethra (Fig. 2).
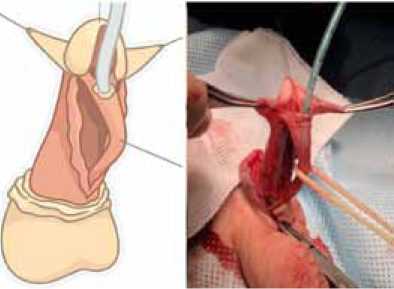
Figure 2. Degloving of the penis. Separation of the urethra from the cavernous bodies with the preserving the integrity of the spongious body
Рисунок 2. Мобилизация кожи полового члена до его основания. Отделение уретры от кавернозных тел с сохранением ножек спонгиозного тела
The length of the distal urethra mobilization from the cavernous bodies depended on diastasis between the misplaced meatus and its physiological position. The distal part of the urethra was separated by 1 cm for every 2 mm of diastasis. The mobilized urethra was moved and the external urethral opening was formed in a physiological rest position on the glans penis (Fig. 3).

Figure 3. Relocating and fixing the urethra in a physiological position
Рисунок 3. Перемещение и фиксация уретры в физиологическом положении
The split distal part of the spongious body was hurled together over the urethra and its anatomy was restored. The relocated urethra was fixed to the cavernous bodies on both sides with the interrupted sutures at 1 cm intervals (Fig. 4).
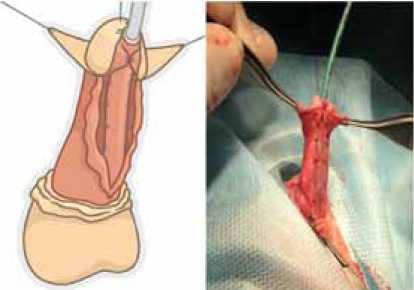
Figure 4. Spongioplasty. Fixing the urethra to the cavernous bodies
Рисунок 4. Спонгиопластика. Фиксация уретры к кавернозным телам
The plastic modelling of the glans penis was performed. The glans penis was hurled together over the advanced distal urethra. The stem part of the urethra was hidden with tunica dartos, thus restoring the normal anatomy of the penis (Fig. 5).
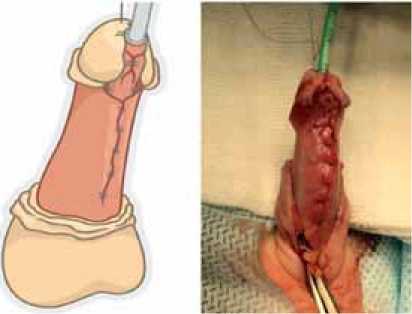
Figure 5. The plastic reconstruction of the glans penis and hiding of the urethra
Рисунок 5. Пластика головки полового члена и укрывание уретры
The plastic surgery of the penile skin was performed and the postoperative wound was sutured layer-by-layer with the formation of interrupted atraumatic sutures (Fig. 6).
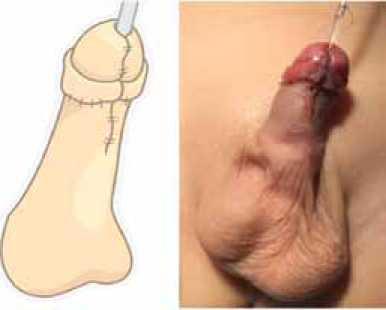
Figure 6. Suturing of the postoperative wound
Рисунок 6. Ушивание послеоперационной раны
A urethral catheter was placed in the urinary bladder. The postoperative wound was covered with an aseptic circular bandage and fixed with an elastic bandage. In 26 cases, the postoperative wound was applied with Histoacryl acrylate glue instead of the circular bandage.
Average values and standard deviation were used as descriptive statistics for quantitative readings, and percentages were used for qualitative ones. Statistical analysis of quantitative readings was performed using the Mann-Whitney test, and the Fischer's Exact test and Pearson criterion (χ2) were used for comparing the qualitative indicators. Statistical processing of results was performed in STATISTICA 12 (StatSoft, Inc, USA).
Results
The postoperative follow-up period lasted 6 - 36 months. All patients were assessed in terms of cosmetic outcomes, early and late postoperative complications.
In the first stage of statistical analysis, groups were compared for comparability by frequency of occurrence of hypospadias various forms (criterion χ2 for arbitrary tables) and age of patients (Mann- Whitney test). In the result of the analysis, no statistically significant differences in the forms of hypospadias and age were revealed, p values were 0.69 and 0.18 respectively.
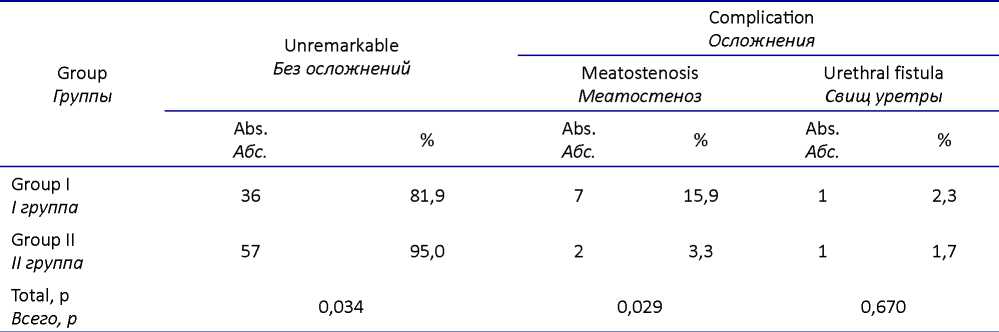
In boys of Group I, the following complications were noted: in seven cases, meatostenosis developed (15.91%) and in one case - urethral fistula (2.27%). Among the patients of Group II from complications requiring surgical treatment were noted two cases of meatal stenosis (3.33%) and one case of urethral fistula (1.67%) (Table).
The total number of complications in the group of comparison was 18.2%, while in the study group it was 5% (p = 0.034). We found that the number of meatostenosises in the study group was 5 times less than in the group of comparison (p = 0.029). Analysis of the urethral fistulas number in both groups showed no differences in the frequency of their formation (p = 0.67).
The cosmetic results obtained after advanced urethroplasty in both groups were identical and were evaluated as good ones by the parents and operating surgeon. Considering the subjectiveness of this criterion assessment, we have not made a statistical assessment of cosmetic results.
Table. Results of surgical treatment
Таблица. Результаты хирургического лечения
Discussion
Convenient in its execution, the technique of advanced urethroplasty in the Beck C.A. modification has some disadvantages from our point of view. Firstly, when the urethra is isolated, it is completely separated from the feeding site, which increases the risk of ischemia of the distal part of the separated urethra, which creates prerequisites for the meatostenosis formation during the postoperative period. Secondly, the dysplastic distal part of urethra separated from the spongiose body of glans penis is not completely covered by the spongiose body of urethra, which increases the risk of urethral fistula developing. Thirdly, when the bifurcated part of the spongious body of the urethra is separated from the glandular part, bleeding occurs, which requires coagulation, and that undoubtedly worsens the blood supply to the moved tissues. all stated above demonstrates the reasons for ischemia of the distal part of mobilized for movement urethra when performing the classic version of the Beck surgery, which creates prerequisites for meatostenosis formation, which is confirmed by publications analyzing the experience of using the Beck technique and reporting a 19.2% frequency of meatostenosis [15].
Our developed modification reduces the risk of distal urethral ischemia after its mobilization, which determines a decrease in the frequency of meatostenosis formation in the series of the presented patients. Our experience shows that an important component of success is the absence of extended dysplasia of the distal part of the urethra. The operation cannot be performed if the distance from the top of the glans penis up to the meatus exceeds 1 cm. In case of wide diastasis, the advancement of the urethra can lead to a secondary curvature of the penis, or, due to tension, it can cause disrupting of the glans and shifting of the meatus to its former place.
Conclusion
Advancement urethroplasty in case of distal hypospadias is advisable for nonextended dysplasia of urethra more proximal of the meatus and the diastasis between the meatus and its physiological rest position, not exceeding 1 cm. Advancement urethroplasty with non-dividing spongioplasty provides a low frequency of meatostenosis formation in the postoperative period compared to the classic Beck technique.
References
1. Snodgrass W. Tubularized, incised plate urethroplasty for distal hypospadias. J Urol. 1994;151(2):464-465. https://doi.org/10.1016/s0022-5347(17)34991-1
2. Lopatkin N.A. eds. Urology. National guide. Moscow: GEOTAR-Media; 2009. (in Russ.).
3. Ashkraft K.U., Holder T.M. Pediatric surgery. Saint-Petersburg: Pit - Tal; 1999: (in Russ.). ISBN 5-90131-10-30
4. Canon S, Mosley B, Chipollini J, Purifoy JA, Hobbs C. Epidemiological assessment of hypospadias by degree of severity. J Urol. 2012;188(6):2362-2366. https://doi.org/10.1016/j.juro.2012.08.007
5. Altarac S, Papes D, Bracka A. Two-stage hypospadias repair with inner preputial layer Wolfe graft (Aivar Bracka repair). BJU Int. 2012;110(3):460-473. https://doi.org/10.1111/j.1464-410X.2012.11304.x
6. Dubrov V.I. Techniques of surgical treatment for hypospadias in boys. Zdravoohranenie. 2011;2:55-58. (in Russ.). eLIBRARY ID: 20397542
7. Beck CA. A new operation for balanic hypospadias. N YMed. J. 1898;67:147.
8. Koff SA. Mobilization of the urethra in the surgical treatment of hypospadias. J Urol. 1981;125(3):394-397. https://doi.org/10.1016/s0022-5347(17)55048-x
9. Awad MM, Tolba AM, Saad KM, Zaghlol MR, Rozigque AE, Gharib O, Khalil SA. What is the best choice for repair of distal penile hypospadias: The tubularized incised plate urethroplasty or anterior urethral advancement technique? Indian J of Plastic Surgery. 2007;40:182-188. https://doi.org/10.4103/0970-0358.37765
10. Alkan M, Oguzkurt P, Ezer SS, Ince E, Hicsonmez A. Evaluation of the results of eccentric circummeatal-based flap with combined limited urethral mobilization technique for distal hypospadias repair. J Pediatr Urol. 2008;4(3):206-209. https://doi.org/10.1016/j.jpurol.2007.11.008
11. Da Silva EA, Sampaio FJ. Urethral extensibility applied to reconstructive surgery. J Urol. 2002;167(5):2042-2045. https://doi.org/10.1097/00005392-200205000-00022
12. Hammouda HM, Hassan YS, Abdelateef AM, Elgammal MA. New concept in urethral advancement for anterior hypospadias. J Pediatr Urol. 2008;4(4):286-289. https://doi.org/10.1016/j.jpurol.2008.01.208
13. Kagancov IM, Akramov NR, Implementing the altered tactics of hypospadias surgery. Prakticheskaja medicina. 2014;9(85):155-159. (in Russ.). eLIBRARY ID: 22597091
14. Patent RF na izobretenie №2684319C2/05.04.2019. Bjul. №10. Akramov N.R., Shavaliev R.F., Filatov V. S., Zakirov A.K., Khaertdinov E.I. Sposob peremeshhajushhej uretro-plastiki s neraschlenjajushhejspongioplastikoj(in Russ) Available at: https://patenton.ru/patent/RU2684319C2 Accessed December 06, 2020.
15. Mouriquand P, Mure PY, Zeidan S, Gelas T. Management of failed hypospadias repairs. In: Azmy AF, Hadidi A, eds. Hypospadias Surgery: An illustrated guide. Berlin: Springer-Verlag; 2003:305-309. https://doi.org/10.1007/978-3-662-07841-943
About the Authors
N. R. AkramovRussian Federation
Nail R. Akramov - M.D., Dr. Sc. (M), Full Prof.; Chief-Researcher, Tatarstan Republican Clinical Hospital; Prof., Dept. of Pediatric Surgery, Kazan SMU.
420064, Republic of Tatarstan, Kazan, 138 Orenburg tract St.; 420012, Republic of Tatarstan, Kazan, 49 Butlerova St., tel.: +7 (917) 253-77-20
Competing Interests: not
I. M. Kagantsov
Russian Federation
Ilya M. Kagantsov- M.D., Dr. Sc. (M), Assoc. Prof. (Docent); Prof., Dept of Surgical Diseases, Pitirim Sorokin SSU; Head, Urological Division.
167001, Komi Republic, Syktyvkar, 55 Oktyabrsky Ave.
Competing Interests: not
V. V. Sizonov
Russian Federation
Vladimir V. Sizonov- M.D., Dr. Sc. (M), Assoc. Prof. (Docent); Prof., Dept. of Urology and Human Reproductive Health(with Pediatric Urology and Andrology Course), Rostov SMU; Head, Pediatric Urology and Andrology Division, Rostov-on-Don Regional Children's CH.
344022, Rostov-on-Don, 14 339th Strelkovoi divizii St.
Competing Interests: not
R. T. Batrutdinov
Russian Federation
Ruslan T. Batrutdinov - M.D., Cand. Sc.(M); Pediatric Urologist, Urology Division.
199053, St. Petersburg, Vasilievsky Island, 47 2-Ln.
Competing Interests: not
V. I. Dubrov
Russian Federation
Vitaly I. Dubrov - M.D., Cand.Sc. (M); Head, Urology Division.
220020, Minsk, 17 Narochanskaya St.
Competing Interests: not
E. I. Khaertdinov
Russian Federation
Elmir I. Khaertdinov - M.D.; Postgraduate, Dept. of Pediatric Surgery, Kazan SMU; Pediatric Surgeon, Tatarstan Republican Children's CH.
420012, Republic of Tatarstan, Kazan, 49 Butlerova St.; 420138, Republic of Tatarstan, Kazan, 140 Orenburg tract St.
Competing Interests: not
Review
For citations:
Akramov N.R., Kagantsov I.M., Sizonov V.V., Batrutdinov R.T., Dubrov V.I., Khaertdinov E.I. Advancement urethroplasty for distal hypospadias repair without dismembering urethra spongy body and glans penis. Urology Herald. 2020;8(3):5-12. https://doi.org/10.21886/2308-6424-2020-8-3-5-12













































