Scroll to:
A rare case of seminoma metastasis to the bladder
https://doi.org/10.21886/2308-6424-2025-13-2-119-122
Abstract
Introduction. The great majority of testis neoplasms are germ cell tumours. The most common site of metastasis is the retroperitoneal region. Metastasis to the bladder is very rare.
Clinical case. A 33-year-old male smoker had right radical orchiectomy two years ago for seminoma. The investigations then showed right retroperitoneal and iliac enlarged nodes and right renal hydronephrosis. Nephrostomy tube was inserted, chemotherapy was given with good response. Two years later the patient presented with right flank pain, hematuria and lower urinary tract symptoms. MRI showed a big bladder mass. Cystoscopy and transurethral resection were done and showed metastatic seminoma.
Discussion. Testicular tumours are the most common male malignant neoplasms between the ages of 15 and 35 years. The great majority of testicular neoplasms are germ cell tumours and seminomas are the most common type of this group. Urinary system metastasis is quite rare.
Conclusion. Rare and late metastases to the bladder should always be considered, and careful medical history should be taken.
For citations:
Al-Tawil M. A rare case of seminoma metastasis to the bladder. Urology Herald. 2025;13(2):119-122. https://doi.org/10.21886/2308-6424-2025-13-2-119-122
Introduction
Testicular tumours are rare, but still the most common malignant tumour in males between 15 and 35 years [1]. The great majority of testis neoplasms are germ cell tumours and seminomas make up about 40% of this group [2]. The most common site of metastasis is the retroperitoneal region, followed by the mediastinum, the lungs, the brain and solid organs, and the bones [3]. Approximately 5% of germ cell tumours originate at extragonadal sites, most commonly mediastinum and retroperitoneum. Testicular tumour metastasis to the bladder is very rare [4].
Case presentation
A 33-year-old male smoker had right radical orchiectomy 2 years ago for seminoma. The investigations then showed right retroperitoneal and iliac enlarged nodes and right renal hydronephrosis. Double-J ureteral stenting failed so nephrostomy tube was inserted, chemotherapy was given with good response. Two years later the patient presented with right flank pain, hematuria and lower urinary tract symptoms. Tumour markers were normal, MRI showed a big bladder mass. Cystoscopy and transurethral resection were done and showed metastatic seminoma. The diagnosis of seminoma was supported by strong immunostaining of the tumour cells for C-Kit and placental alkaline phosphatase. Salvage chemotherapy (four cycles of cisplatin and ifosfamide + etoposide) was given and cystoscopic follow-up showed normal bladder.
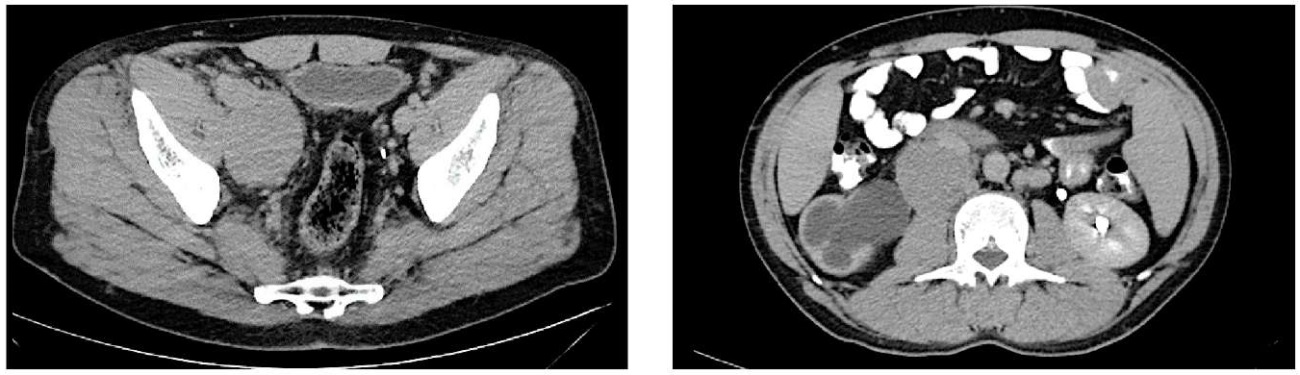
Figure 1. CT axial scans showing right retroperitoneal and iliac enlarged nodes and right renal hydronephrosis [the first presentation
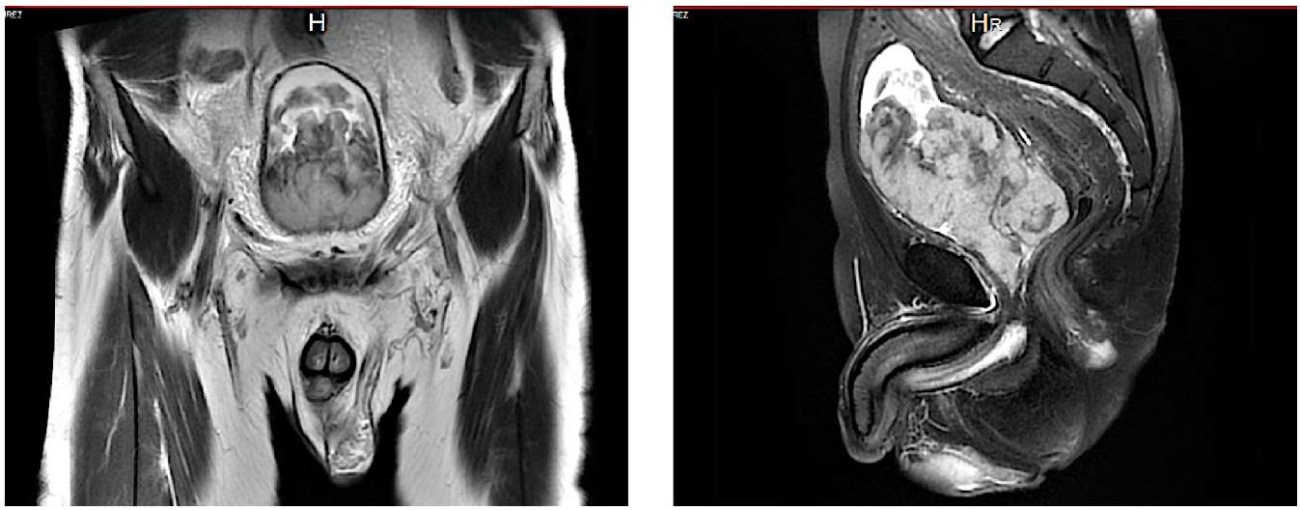
Figure 2. MRI scans (left — sagittal, right — coronal) showing the bladder mass [the second presentation]
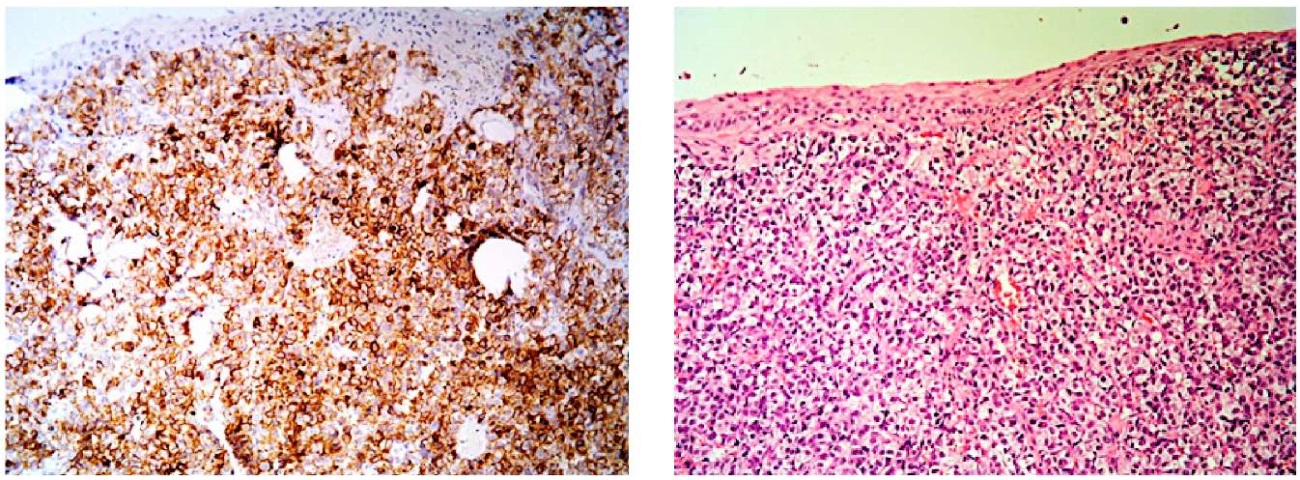
Figure 3. Bladder biopsies showing seminoma (left — H&E staining, right — IHC staining)
Discussion
More than 95% of testicular neoplasms are germ cell tumours, which contain seminoma, non-seminoma and mixed tumours. Germ cell tumours (GCTs) are a relatively rare malignancy, accounting for 1% to 2% of cancers among adult males [1].
About 95% of germ cell tumours arise in the testis, approximately 5% of postpubertal GCTs are extragondal in origin, and most develop in midline anatomic locations (retroperitoneum and mediastinum are most common) [2]. With the development of cisplatin-based chemotherapy and the integration of surgery, GCTs have become a model of a curable neoplasm and serve as a paradigm for the multidisciplinary treatment of cancer [5]. Currently, the long-term survival for men with metastatic GCT is 80% to 90% [6].
The most common presentation of testis cancer is a painless testis mass.
Regional or distant metastasis at diagnosis is present in approximately two-thirds of NSGCTs and 15% of pure seminomas, and symptoms related to metastatic disease are the presenting complaint in 10% to 20% of patients [7]. Bulky retroperitoneal metastasis may cause a palpable mass, abdominal or flank pain, or lower extremity swelling. Testis cancer is associated with serum tumour markers (LDH, AFP, and beta-HCG) that are essential in its diagnosis and management. Seminomas do not produce AFP. Serum tumour marker levels should be obtained at diagnosis, after orchiectomy, to monitor for response to chemotherapy.
Similar reported cases include: A.R. Türkoğlu et al. (2015) reported a case of rare late metastasis of testicular seminoma to the bladder [8], Y.S. Gürbüz et al. (2001) reported a case with simultaneous bladder carcinosarcoma and testicular seminoma [9]. A. Alsolamı et al. (2014) reported a case with concurrent bladder and testicular seminoma [10]; Another patient was diagnosed with extragonadal germ cell tumour with lymph node biopsy after retroperitoneal and cervical lymphadenopathy was detected, Chemotherapy was administered and the beta-HCG level increased during follow-up, The patient developed hematuria with bladder and right ureter metastasis followed by liver and mesenteric lymph node metastasis leading to his death [11]. Another case is present where orchiectomy was performed for testis seminoma and biopsy of the paraaortic and inguinal lymph nodes during a kidney transplant later in this kidney recipient revealed seminoma again. The patient underwent radiotherapy and received immunosuppressives, but a bladder metastatic seminoma was found three years later [12]. Another article reported a patient who underwent bilateral orchiectomy, retroperitoneal lymph node dissection, and chemotherapy for seminoma; the patient then developed a retrovesical 8 × 6 × 5 cm primary seminoma of the prostate 16 years later [13]. J.D. Khandekar et al. (1993) reported a case involving the prostate and bladder neck [14]. T. Hashimoto et al. (2009) reported a primary seminoma involving the prostate [15]. Renal, adrenal gland, psoas muscle, gastric, seminal vesicle, bladder, prostate and pericardial involvement are very rare (< 1%) [4]. Most metastases develop within the first two years [7].
Conclusion
Rare and late metastases to the bladder should always be considered, and careful medical history should be taken.
References
1. Znaor A, Skakkebaek NE, Rajpert-De Meyts E, Kuliš T, Laversanne M, Gurney J, Sarfati D, McGlynn KA, Bray F. Global patterns in testicular cancer incidence and mortality in 2020. Int J Cancer. 2022;151(5):692- 698. DOI: 10.1002/ijc.33999
2. Richie JP, Steele GS. Neoplasms of the testis. In: Kavaoussi LR, Novick AC, Partin AW, Peters CA, eds. Campbell-Walsh Urology. 9th ed. Philadelphia: Saunders; 2007.
3. McKenney JK, Heerema-McKenney A, Rouse RV. Extragonadal germ cell tumors: a review with emphasis on pathologic features, clinical prognostic variables, and differential diagnostic considerations. Adv Anat Pathol. 2007;14(2):69-92. DOI: 10.1097/PAP.0b013e31803240e6
4. Husband JE, Bellamy EA. Unusual thoracoabdominal sites of metastases in testicular tumors. AJR Am J Roentgenol. 1985;145(6):1165-1171. DOI: 10.2214/ajr.145.6.1165
5. Chaganti RS, Houldsworth J. Genetics and biology of adult human male germ cell tumors. Cancer Res. 2000;60(6):1475-1482. PMID: 10749107.
6. Einhorn LH. Testicular cancer as a model for a curable neoplasm: The Richard and Hinda Rosenthal Foundation Award Lecture. Cancer Res. 1981;41(9 Pt 1):3275-3280. PMID: 6167346.
7. Albers P, Albrecht W, Algaba F, Bokemeyer C, Cohn-Cedermark G, Fizazi K, Horwich A, Laguna MP; European Association of Urology. EAU guidelines on testicular cancer: 2011 update. Eur Urol. 2011;60(2):304- 319. DOI: 10.1016/j.eururo.2011.05.038
8. Türkoğlu AR, Coban S, Guzelsoy M, Demirbas M, Mutlu N, Yalcin O. Rare late metastasis of testis seminoma to the bladder. Can Urol Assoc J. 2015;9(11-12):E823-E825. DOI: 10.5489/cuaj.3250
9. Gürbüz YS, Müezzinoglu B, Cimen K, Dillioglugil O. Synchronous occurrence of bladder carcinosarcoma and testicular seminoma. Int J Urol. 2001;8(7):404-407. DOI: 10.1046/j.1442-2042.2001.00322.x
10. Alsolami A, Alotaıbı M, Bazarbashı S, Almutawa A, Akhtar M. Seminoma presenting as a polypoid bladder mass: a case report. Turk Patoloji Derg. 2014;30(1):69-72. DOI: 10.5146/tjpath.2013.0120
11. Nakatani T, Sugimura K, Naganuma T, Kamikawa S, Sugimoto T. Metastatic urinary bladder tumor from extragonadal germ cell tumor: a case report. Oncol Rep. 2002;9(6):1209-1211. PMID: 12375021.
12. Viddeleer AC, Lycklama à Nijeholt GA, Beekhuis-Brussee JA. A late manifestation of testicular seminoma in the bladder in a renal transplant recipient: a case report. J Urol. 1992;148(2 Pt 1):401-402. DOI: 10.1016/s0022-5347(17)36611-9
13. Alsharif M, Aslan DL, Jessurun J, Gulbahce HE, Pambuccian SE. Cytologic diagnosis of metastatic seminoma to the prostate and urinary bladder: a case report. Diagn Cytopathol. 2008;36(10):734-738. DOI: 10.1002/dc.20881
14. Khandekar JD, Holland JM, Rochester D, Christ ML. Extragonadal seminoma involving urinary bladder and arising in the prostate. Cancer. 1993;71(12):3972-3974. DOI: 10.1002/1097-0142(19930615)71:12<3972::aid-cncr2820711228>3.0.co;2-p
15. Hashimoto T, Ohori M, Sakamoto N, Matsubayashi J, Izumi M, Tachibana M. Primary seminoma of the prostate. Int J Urol. 2009;16(12):967- 970. DOI: 10.1111/j.1442-2042.2009.02403.x
About the Author
Muhamad Al-TawilSyrian Arab Republic
Muhamad Al-Tawil — MD, PhD, Assoc.Prof.
Damascus
Competing Interests:
The author declares no conflict of interest.
Review
For citations:
Al-Tawil M. A rare case of seminoma metastasis to the bladder. Urology Herald. 2025;13(2):119-122. https://doi.org/10.21886/2308-6424-2025-13-2-119-122
JATS XML













































