Scroll to:
Transurethral balloon dilation safety and efficacy in patients with recurrent bladder neck contracture after transurethral interventions
https://doi.org/10.21886/2308-6424-2024-12-4-5-13
Abstract
Introduction. Currently, urologists are divided on which method is most effective for treating bladder neck contracture (BNC) after surgery: transurethral resection (TUR) or incision.
Objective. The study aimed to assess the balloon dilation safety and success in patients with recurrent bladder neck contracture (BNC) after endoscopic surgery for benign prostatic hyperplasia (BPH).
Materials & Methods. This study involved 110 patients with recurrent BNC after transurethral interventions for BPH. All patients underwent TUR of the bladder neck and were divided into 2 groups: group A (n = 45) included men who, after TUR, additionally underwent repeated balloon dilation, while the control group B (n = 65) included men who were treated with alpha-blockers alone.
Results. In 9 months after TUR and 3 months after the fourth balloon dilation procedure in group A, the mean international prostate symptom score (IPSS) decreased from 20.1 ± 8.4 to 17.2 ± 7.4, and the IPSS-quality of life (QoL) was 4.2 ± 1.2 (p > 0.05). In group B, they were 21.7 ± 7.7 and 4.7 ± 1.1 (p > 0.05), respectively. Additionally, the mean flow rate in group A was 13.2 ± 5.4 ml/s, while in group B, it was 8.7 ± 4.9 ml/s (p < 0.05). There was a significant decrease in the post-void residual urine volume (PVR) from 76.2 ± 96.1 ml to 37.6 ± 55.1 ml in group A, whereas, in group B, it increased from 63.0 ± 36.9 ml to 79.4 ± 71.6 ml (p > 0.05). Also, 28.0% of patients of group B, and 13.3% of patients of group A underwent repeated TUR of the bladder neck in 9 months follow-up period (p < 0.05).
Conclusion. Balloon dilation procedure is a relatively safe less invasive procedure and can reduce the BNC recurrence rate and consequently the rate of repeated transurethral interventions.
Keywords
For citations:
Abbosov Sh.A., Shomarufov A.B., Aminova D.R. Transurethral balloon dilation safety and efficacy in patients with recurrent bladder neck contracture after transurethral interventions. Urology Herald. 2024;12(4):5-13. https://doi.org/10.21886/2308-6424-2024-12-4-5-13
Introduction
Transurethral resection of the prostate (TURP) and endoscopic enucleation is currently considered the most effective [1 – 6], mastered, and available standards of surgical correction of bladder outlet obstruction [7]. The operation has been used in clinical practice for more than 50 years and is recognized as an effective, relatively safe method of treating patients with benign prostatic hyperplasia (BPH) of medium size and is accompanied by a small number of such short term postoperative complications as minor bleeding (is observed in approximately 1.7% to 8.2% of cases), and TUR syndrome (occurs in up to 1.1% of cases) and a short length of hospital stay [4][8]. Nevertheless, the long-term sclerotic changes in the bladder neck that occur after endoscopic procedures on the prostate require repeated surgical interventions, which significantly reduce the quality of life of patients and negatively affect the state of the male genitourinary system.
It should be noted that with TURP performed in a small volume of BPH, complications occur in 15% of cases and include bleeding, urethral stricture (which is detected in 2.2 – 9.8% of cases), and subsequent sclerosis (ranging from 0.3% to 9.1% of cases) [9 – 11]. One of the reasons for the fibrosis the formation is the extended resection of tissues in the bladder neck, which can be the cause of narrowing or deformity [12].
The treatment of sclerosis is a difficult task [13], even for experienced urologists, as often several interventions have to be performed to correct the bladder outlet obstruction [14]. As a rule, the following endoscopic methods are used: dilation, image-guided urethrotomy, and bladder neck resection. After such interventions, urinary incontinence is common, which worsens the quality of life of patients [15][16].
Currently, there is no consensus among urologists regarding which method is advisable for postoperative stricture of the posterior urethra / bladder neck (bladder neck contracture — BNC): TUR or incision. Therefore, we aimed to assess the results of transurethral balloon dilation of the bladder neck in patients with recurrent BNC after endoscopic surgeries for BPH.
Materials and Methods
Study Design. This prospective non-randomized multicentre study was approved by the Institutional Local Ethical Committees of Medical Research and Educational Centre of Lomonosov Moscow State University (MREC, Moscow, Russia) (№ 1/21 from 25.01.2019) and the Republican Specialized Scientific and Practical Medical Centre of Urology (RSSPMCU, Tashkent, Uzbekistan) (№ 6 from 01.08.2021) which was conducted following the Declaration of Helsinki and the Good Clinical Practice guidelines. All patients signed an appropriate informed consent.
Patients. In total 173 patients underwent TURP and laser enucleation underwent TUR underwent TUR of the bladder neck using electro- (bipolar) and laser energy during the period from April 2019 to August 2022 at the MREC and RSSPMCU.
The criteria for the inclusion of patients in the study were the presence of BNC formed after TURP and endoscopic enucleation of the BPH.
35 patients who underwent surgeries for malignant neoplasms of the prostate were excluded from the study. 13 patients were excluded because of post-traumatic urethral strictures and 15 patients were excluded because of post-inflammatory urethral strictures. As a result, 110 patients were included in our study. After the intervention, the patients were randomized into two groups: group A (n = 45) included men who additionally underwent transurethral balloon dilation after TUR of the bladder neck, while control group B (n = 65) included men who received conservative therapy alone with alpha-blockers (tamsulosin 0.4 mg o.d.).
All patients, in addition to routine clinical and laboratory studies, underwent uroflowmetry before surgery, and the volume of residual urine (PVR) was also measured. Transrectal ultrasonography (TRUS) of the prostate was performed. Narrowing (sclerosis) of the bladder neck was confirmed by urethrocystoscopy (Fig. 1).
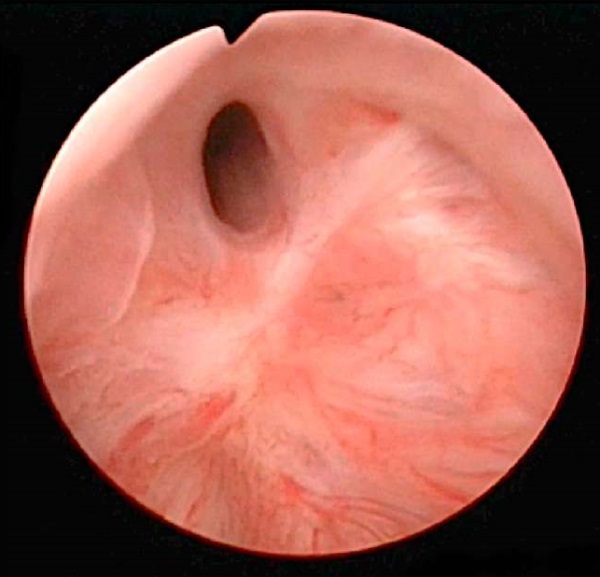
Figure 1. Cystoscopic view of bladder neck contracture
Balloon dilation technique. To assess the condition of the bladder neck before balloon dilation, prostate TRUS was performed, and the condition of the prostate was assessed by visualizing it in a longitudinal and cross-section. For the transrectal ultrasound diagnostic system, EPIQ 7 (Koninklijke Philips N.V. — Philips Medical Systems Nederland B.V., Heerlen, The Netherlands) with an intracavitary probe (4 – 10 MHz) was utilized. The length of the bed of the removed BPH, the anteroposterior dimension in the widest part, the bilateral dimension in the widest part, the volume of the defect, and the anteroposterior dimension of the bladder neck were measured (Fig. 2).
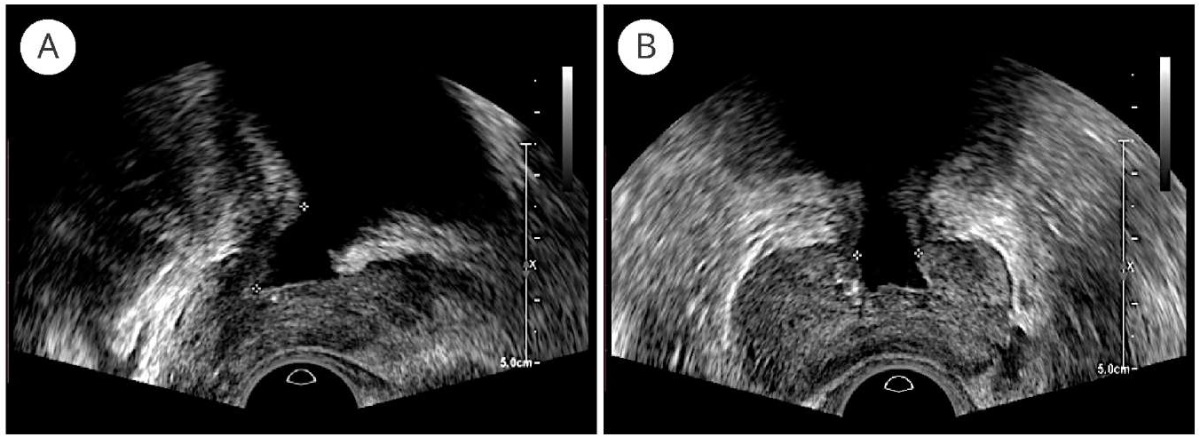
Figure 2. TRUS picture of the prostate and bed of the removed BPH:
A — longitudinal section; B — cross-section
After the introduction of Cathejell® with Lidocaine 12.5 gr. anesthetic gel into the urethra, a balloon-type urethral catheter — 3-way Dufour Rusch® SoftSimplastic (Teleflex Medical Europe, Ltd., Dublin, Ireland) with an increased capacity was inserted through the urethra into the lumen of the bladder. The best approach, in our opinion, for this procedure is an 18 Fr balloon catheter, the diameter of which allows it to pass through the narrowed part of the urethra and the elasticity of which is sufficient to dilate the fibrotic ring of the bladder neck. Balloon dilation was performed with a bladder volume of at least 150 ml.
Under TRUS control, the balloon of the urethral catheter was placed into the lumen of the bladder neck so that the widest part of the balloon was localized around the fibrotic ring of the bladder neck and inflated to a size slightly larger than the diameter of the bed of the removed BPH so that the walls of the balloon exerted pressure on the fibrotic ring. The balloon was left in this position for 5 minutes, during which, due to the property of elasticity, the balloon tended to take the shape characteristic of the inflated state and eliminate the compression, due to which gentle elastic stretching and tearing of the fibrotic ring of the bladder neck occurred. Next, a similar manipulation was performed by moving the balloon to the bed of the removed BPH (Fig. 2). Then the balloon was completely deflated and removed from the bladder cavity. The approximate procedure duration was 15 – 20 minutes.
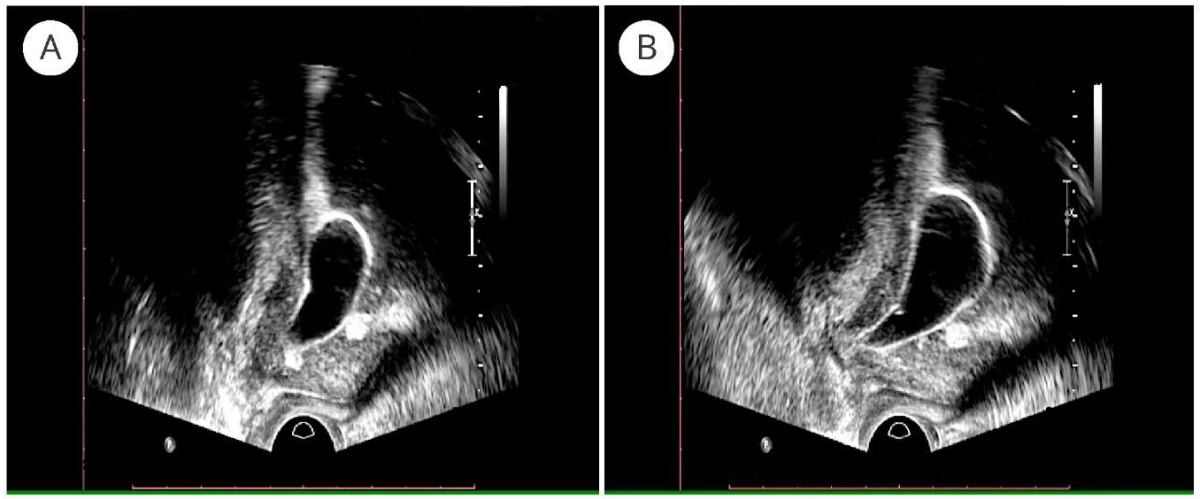
Figure 3. TRUS guided balloon dilation procedure
(arrow — balloon of the catheter located around the bladder neck fibrotic ring):
A — after the inflation of the balloon (5 ml); B — after the 5-minute exposition
To evaluate the results of the performed procedure, the measurements of the length of the removed BPH bed, the anteroposterior size in the widest part, the bilateral size in the widest part, the anteroposterior size, and the volume of the bladder neck defect were repeated. The results of both measurements reflect the state of the neck before and after the manipulation, that is, they visualize the dilating effect of the procedure. This study allowed us to assess the individual dynamics of the functional state of the bladder neck according to the above indicators. After the completion of the manipulation, uroflowmetry was performed to control the urodynamic status of the patient.
Recurrence of BNC was defined as decreased urinary flow rate, incomplete bladder emptying, increased PVR, the obstructive pattern on the uroflow study, increased IPSS-score.
Balloon dilation was performed in several sessions until the desired effect was obtained, and the results of stretching the bladder neck were consolidated. The patient underwent repeated balloon dilation interventions in 1, 2, 3, and 6 months after TUR of the bladder neck.
Statistical Analysis. Statistical data analyzed in MS Excel 2016 Microsoft Office Excel 365 (Microsoft Corp., Redmond, WA, USA) and IBM SPSS© Statistics 20.0 (SPSS: An IBM Company, IBM SPSS Corp., Armonk, NY, USA) statistical packages. The analysis of the obtained values distribution normality was carried out according to the one-sample Kolmogorov-Smirnov Z criterion. When a distribution is normal, the mean values for the groups are presented as a sample mean value and standard deviation — M (S), and when it differs from normal, as a median with 25 – 75% quartiles. The significance of differences between groups is calculated using Students (t) tests for means, Mann-Whitney, and Wilcoxon for medians and ranks; differences are considered significant at p < 0.05.
Results
Patients and Treatment. In total 110 patients were randomly divided into group A (n = 45) men who underwent balloon dilation after TUR, and control group B (n = 65) men who received conservative therapy only.
The main baseline clinical and anamnestic characteristics of the patients are shown in table 1.
Table 1. Baseline clinical parameters of patients
|
Groups |
Mean age, years |
Body mass index, kg/m² |
Prostate volume (before BPH surgery), cm³ |
Urinary tract infections, n (%) |
Number of prior interventions, mean ± SD |
Type 2 diabetes mellitus, n (%) |
Ischemic heart disease, n (%) |
|
Group А (n = 45) |
65.7 ± 11.6 |
27.3 ± 3.9 |
40.7 ± 9.3 |
28 (62.2%) |
2.2 ± 1.1 |
9 (20%) |
16 (35.5%) |
|
Group B (n = 65) |
63.7 ± 12.8 |
25.6 ± 7.5 |
42.4 ± 10.9 |
43 (66%) |
2.7 ± 2.4 |
14 (21.5%) |
28 (43%) |
|
Р |
> 0.05 |
> 0.05 |
> 0.05 |
> 0.05 |
> 0.05 |
> 0.05 |
> 0.05 |
Clinical Outcome. In 1 month after the 1st balloon dilation procedure, the main parameters (uroflowmetry, PVR, IPSS, IPSS-QoL) of the patients of group A improved significantly (p < 0.05 for all). There was a statistically significant difference between groups after treatment in all parameters, except for IPSS (Tabl. 2), i.e. in patients of group A, these parameters were significantly better.
Table 2. Dynamics of some parameters in the groups
after balloon dilation of the bladder neck
|
Groups |
Indicators |
Before |
Check-up 1* |
Check-up 2* |
Check-up 3* |
Check-up 4* |
|
Group A (n = 45) |
IPSS |
20.1 ± 8.4 |
13.4 ± 5.8** |
14.5 ± 6.2 |
13.7 ± 7.9** |
17.2 ± 7.4** |
|
IPSS-QoL |
4.4 ± 1.0 |
2.7 ± 0.8** |
3.4 ± 1.2** |
3.4 ± 1.3** |
4.2 ± 1.2** |
|
|
Q max (ml/s) |
7.8 ± 2.9 |
14.6 ± 4.4 |
12.1 ± 3.1 |
10.1 ± 3.1 |
13.2 ± 5.4** |
|
|
PVR (ml) |
76.2 ± 96.1 |
15.8 ± 12.7** |
16.7 ± 11.5** |
31.3 ± 36.9* |
37.6 ± 55.1** |
|
|
Group B (n = 65) |
IPSS |
18.6 ± 6.7 |
16.7 ± 6.1 |
16.8 ± 6.5 |
19.0 ± 8.4 |
21.7 ± 7.7 |
|
IPSS-QoL |
4.2 ± 0.9 |
3.7 ± 0.7 |
4.4 ± 1.1 |
4.3 ± 1.1 |
4.7 ± 1.1 |
|
|
Q max (ml/s) |
8.2 ± 4.3 |
13.7 ± 6.1 |
10.7 ± 4.9 |
8.9 ± 4.5 |
8.7 ± 4.9 |
|
|
PVR (ml) |
63.0 ± 36.9 |
33.7 ± 22.6 |
56.7 ± 84.5 |
65.2 ± 46.7 |
79.4 ± 71.6 |
Note. * Check-up 1 – 2 months after TUR and 1 month after the 1st balloon dilation procedure;
Check-up 2 – 3 months after TUR and 1 month after the 2ed balloon dilation procedure;
Check-up 3 – 4 months after TUR and 1 month after the 3rd balloon dilation procedure;
Check-up 4 – 9 months after TUR and 3 months after the 4th balloon dilation procedure;
** — p < 0.05, between Group A and B
However, a slight worsening of the studied parameters was observed in group A beginning from 3 months after the TUR and this tendency saved till the end of the follow-up. But in comparison with the parameters of patient of the group B given worsening was not so significant. Significant deterioration in 3 months after TURP developed in 4 (8.8%) patients in group A, whereas in group B, deterioration was observed in 12 (18,5%) patients (p < 0.05). This indicator was 20% (9 patients) and 35% (23 patients) in groups A and B after 9 months, respectively (p < 0.05).
In 9 months after TURP of the bladder neck and 3 months after the 4th balloon dilation, the average maximum urine flow rate in group A was 13.2 ± 5.4 ml/s, while in group B this parameter was 8.7 ± 4.9 ml/s. Also, in group A, a significant decrease in the PVR was revealed — from 76.2 ± 96.10 to 37.6 ± 55.1 ml, and in group B this indicator decreased from 63.0 ± 36.9 to 79.4 ± 71.6 ml (Tabl. 2).
During the follow-up period, recurrence of BNC developed in 27 patients (24.5%) of both groups. All of them underwent repeated TUR of the bladder neck. In 8 patients (7 from group B, 1 from group A) recurrence was observed in 3 months after TUR. In 12 patients (9 from group B, 3 from group A) recurrence developed after 6 months, whereas in 7 patients (5 from group B, 2 from group A) BNC recurred after 9 months. The main parameters of the patients with BNC recurrence are given in table 3.
Table 3. Parameters in the groups after balloon dilation of the bladder neck,
who had a recurrence
|
Groups |
Rate (%) |
IPSS |
IPSS-QoL |
Q max (ml/s) |
PVR (ml) |
|
Group A (n = 45) |
6 (13.3%) |
31.33 + 1.63 |
5.33 + 1.21 |
2.96 + 0.61 |
169.17 + 42.24 |
|
Group B (n = 75) |
21 (32.3%) |
29.89 + 0.61 |
5.14+0.15 |
3.35 + 0.17 |
187.38 + 27.69 |
|
P |
> 0.05 |
>0.05 |
> 0.05 |
> 0.05 |
Adverse Events and Complication Rates. Balloon dilation procedures were accompanied by a less amount of light to moderate complications. Acute urinary retention developed only in 1 (2.2%) case, which was resolved with indwelling catheterization for 48 hours. In 2 (4.4%) patients acute orchiepididymitis was observed and treated successfully with antibacterial drugs. In 14 (31.1%) men in group A, haematuria was determined, which did not require the use of hemostatic drugs and was not accompanied by a decrease in haemoglobin in the peripheral blood, in 4 (8.8%) patients’ short-term urethrorrhagia occurred which resolved without additional therapy. Dysuria was observed in 8 (17,8%) patients, which resolved without treatment. There were no severe surgical complications in group A according to the Clavien-Dindo scoring system that required repeated intervention during the 90-day postoperative period.
Discussion
Despite the fact that, in recent years, new endoscopic methods of treatment of patients with BPH have been developed and introduced into practice, including bipolar resection (B-TURP) and laser enucleation, the complications’ rate after these surgical interventions remains quite high, including the urethral strictures (2.2 – 9.8%) and BNC (0.3 – 9.2%) [15]. Contracture of the bladder neck significantly worsens the long-term results of TURP and the quality of life of patients, who often undergo repeated and painful surgical interventions without obtaining the desired result. Therefore, the treatment of this category of patients is a serious clinical problem, which is reflected in the fact that various methods of treatment are proposed, such as deep lateral incisions of the urethral wall using a cold knife or laser, bipolar vaporization of the bladder neck, an incision with an intravesical injection of mitomycin C and T-plasty, and finally, balloon dilation and reconstructive surgery [17]. However, all of these methods of treatment are associated with a significant frequency of relapses, and urologists continue to search for the best method, preferably minimally invasive, to eliminate postoperative BNC. In this light, a promising direction is the application of the balloon dilation technique, which is successfully used in practice as an alternative method of treating urethral strictures. To our knowledge, we are the first contributors to the evidence for this method application.
It is believed that sclerosis usually occurs after resections performed on the small prostate (< 30 g) and that such sclerosis is a consequence of tissue ischemia [9][15]. Therefore, the indications for performing TURP in cases of small prostate size should be treated very cautiously. In our study, the mean prostate size was also small (41,5 ± 9,3 g).
Steenkamp et al. studied the results of using dilation and internal urethrotomy as a treatment for postoperative urethral strictures. The authors did not find a significant difference in the effectiveness of the methods used; however, they emphasized that the procedures are less effective with an increase in the length of the stricture and recommend dilation or internal optical urethrotomy for strictures no more than 2 cm in length. In this observation, the recurrence rate 12 months after the intervention was approximately 40% in patients with urethral strictures less than 2 cm in length and 80% in patients with a length of 4 cm [18]. According to our results, the recurrence rate of BNC was 24,5% (27 out of 110) during 9 months follow-up.
Transurethral balloon dilation is easy to perform and less invasive than cold knife incision, and the advantage of balloon dilation is the lower risk of urethral injury. The most frequent complications, which can occur in up to 20% of cases after urethrotomy, are perineal hematomas and bleeding from the urethra, which requires additional interventions [18][19]. It is also should be noted that urinary incontinence is observed in 75% of cases [17]. No cases of urinary incontinence and perineal hematomas were revealed during our study.
The most expedient, easily feasible, and affordable way of eliminating postoperative bladder outlet obstruction is the use of a special catheter with a balloon that allows an increase in the lumen of the urethra [20]. However, the conditions for using this method in the treatment of patients with BNC are the presence of a preserved lumen and the absence of extended urethral strictures. Therefore, when using this method, before the operation, all patients undergo urethrography and urethroscopy to determine the state of the urethra and bladder and the possibility of using balloon dilation. Dilation is usually fast, gives immediate results, and is technically relatively easy to manipulate. It should be noted that dilation involves sequential stretching rather than rupture of the stricture tissue.
There are a lot of reports dedicated to endoscopic balloon dilation of bladder neck around vesicourethral anastomosis after radical prostatectomy [21]. Park et al. reported about 93% of success in 24 patients during at least 12 months [22]. Transurethral balloon dilation also was performed by Ramchandani et al. in patients with postoperative stricture of the prostatic urethra after radical prostatectomy and was successful in 59% (mean, 31.5 months 7 years to 12 months) of cases; the rest of the patients underwent transurethral dissection of the bladder neck. Later, however, these men required a redo of balloon dilation. The author noted that urinary incontinence was found only in one patient who underwent incision of the bladder neck, and no case of incontinence was found in those who underwent balloon dilation [23]. According to our data, the treatment success rate was 87% during 9-month period and no cases of urinary incontinence were observed.
However, Ramchandani used a “low” pressure cylinder. Ishii used a high-pressure urethral balloon catheter (up to 30 atm) to treat patients with postoperative strictures, which provided a sufficient increase in its volume and led to dilation of the narrowing. It is not clear at this time whether the higher pressure in the balloon is a positive factor, and the expansion is more efficient than using a “regular” balloon. However, on the positive side, forces are applied radially to expand the stricture while avoiding the potentially traumatic moments associated with sequential rigid dilation. The use of this method made it possible to achieve positive results in 80% of cases [24]. We also used a high-pressure urethral catheter (up to 4.9 atm), which made it possible to overcome the resistance of the scar tissue of the bladder neck.
Gelman et al. reported that they applied dilation using a rigid cystoscope, and the position of the balloon was visually monitored. The authors believe that because the procedure is performed with direct imaging, it is more controllable than using wires and avoids false path formation. However, the intervention requires general or spinal anesthesia, and after surgery, there is a need for hospitalization of the patient [25]. The balloon dilation technique we proposed can be performed under TRUS guidance using local anesthetics on an outpatient basis.
Therefore, Vyas et al. retrospectively studied the results of balloon dilation performed in patients with urethral strictures after endoscopic and traditional operations. Patients with stricture lengths less than 1.5 cm were treated under X-ray control. A balloon catheter (Cook Urological, Spencer, Indiana) was inserted into the urethra via a metal guide and pressurized in the balloon until the waist disappeared. It should be noted that we also focused on balloon deformation; however, we performed dilation in two areas, while the abovementioned authors used balloon dilation in one position. After the intervention, the bladder was drained using a urethral catheter, as in our case. The stricture was eliminated in 68.3% of patients [26].
Xie et al. used balloon dilation of urethral strictures under ultrasonographic control. The operation was performed successfully in all patients without any major complications. The urethral catheter was removed 3 – 4 weeks after surgery. However, the method was used in the treatment of 5 patients with urethral strictures; nevertheless, the authors achieved good results, and the effectiveness of the operation was assessed using urethrocystoscopy [27]. We also used ultrasonography for balloon dilation, whereby we measured the length of the bed of the removed prostate, the anteroposterior dimension in the widest part, the bilateral dimension in the widest part, the volume of the defect, and the anteroposterior dimension of the bladder neck. After dilation, the effectiveness of the manipulation was assessed by the comparison method.
Our study has certain limitations like the small size of the sample with patients who underwent balloon dilation and the short follow-up period. Nevertheless, the findings are statistically significant, which suggests that they can be extrapolated to the general sample of patients with BNC. Balloon dilation is a promising less invasive procedure that can be applied on an outpatient basis. Of course, further large-scale and well-organized studies are needed to confirm or reject the clinical value of this treatment method.
Conclusion
- TRUS-guided transurethral balloon dilation procedure is a relatively safe less invasive procedure.
- It can reduce the BNC recurrence rate and consequently the rate of repeated transurethral interventions.
- In some selective cases this method may replace other routine treatment methods such as transurethral incisions or resections.
References
1. Xiang P, Guan D, Du Z, Hao Y, Yan W, Wang Y, Liu Y, Liu D, Ping H. Efficacy and safety of prostatic artery embolization for benign prostatic hyperplasia: a systematic review and meta-analysis of randomized controlled trials. Eur Radiol. 2021;31(7):4929-4946. DOI: 10.1007/s00330-020-07663-2
2. Frendl DM, Chen YW, Chang DC, Kim MM. A Claims Based Assessment of Reoperation and Acute Urinary Retention after Ambulatory Transurethral Surgery for Benign Prostatic Hyperplasia. J Urol. 2021;205(2):532-538. DOI: 10.1097/JU.0000000000001390
3. Arcaniolo D, Manfredi C, Veccia A, Herrmann TRW, Lima E, Mirone V, Fusco F, Fiori C, Antonelli A, Rassweiler J, Liatsikos E, Porpiglia F, De Sio M, Autorino R; EAU Section of Uro-Technology (ESUT) Research Group. Bipolar endoscopic enucleation versus bipolar transurethral resection of the prostate: an ESUT systematic review and cumulative analysis. World J Urol. 2020;38(5):1177-1186. DOI: 10.1007/s00345-019-02890-9
4. Sun F, Sun X, Shi Q, Zhai Y. Transurethral procedures in the treatment of benign prostatic hyperplasia: A systematic review and meta-analysis of effectiveness and complications. Medicine (Baltimore). 2018;97(51):e13360. DOI: 10.1097/MD.0000000000013360
5. Zhang Y, Fu C, Wang J, Wu P, Chen X, Hou H, Song X, Cheng W, Wang J, Liu M. Enucleation of the Prostate for the Treatment of Benign Prostatic Hyperplasia Using a 980 nm Diode Laser. J Vis Exp. 2020;(159). DOI: 10.3791/60532
6. Enikeev D, Rapoport L, Gazimiev M, Allenov S, Inoyatov J, Taratkin M, Laukhtina E, Sung JM, Okhunov Z, Glybochko P. Monopolar enucleation versus transurethral resection of the prostate for small- and mediumsized (< 80 cc) benign prostate hyperplasia: a prospective analysis. World J Urol. 2020;38(1):167-173. DOI: 10.1007/s00345-019-02757-z
7. Reale G, Marchioni M, Altieri V, Greco F, De Nunzio C, Destefanis P, Ricciardulli S, Bergamaschi F, Fasolis G, Varvello F, Voce S, Palmieri F, Divan C, Malossini G, Oriti R, Tuccio A, Ruggera L, Tubaro A, Delicato G, Laganà A, Dadone C, De Rienzo G, Ditonno A, Frattini A, Pucci L, Carrino M, Montefiore F, Germani S, Miano R, Schips L, Rabito S, Ferrari G, Cindolo L. Operative profile, safety and functional outcomes after GreenLight laser prostate surgery: results from a 12 months follow-up multicenter Italian cohort analyses. Minerva Urol Nefrol. 2020;72(5):622-628. DOI: 10.23736/S0393-2249.20.03597-3
8. Ibrahimi A, Ziani I, El Boukili El Makhoukhi Z, El Sayegh H, Benslimane L, Nouini Y. Transurethral resection syndrome: A rare complication of intraperitoneal bladder perforation during transurethral resection of bladder tumor. Urol Case Rep. 2020;34:101465. DOI: 10.1016/j.eucr.2020.101465
9. Rassweiler J, Teber D, Kuntz R, Hofmann R. Complications of transurethral resection of the prostate (TURP)--incidence, management, and prevention. Eur Urol. 2006;50(5):969-979; discussion 980. DOI: 10.1016/j.eururo.2005.12.042
10. Ahyai SA, Gilling P, Kaplan SA, Kuntz RM, Madersbacher S, Montorsi F, Speakman MJ, Stief CG. Meta-analysis of functional outcomes and complications following transurethral procedures for lower urinary tract symptoms resulting from benign prostatic enlargement. Eur Urol. 2010;58(3):384-397. DOI: 10.1016/j.eururo.2010.06.005
11. Grechenkov A, Sukhanov R, Bezrukov E, Butnaru D, Barbagli G, Vasyutin I, Tivtikyan A, Rapoport L, Alyaev Y, Glybochko P. Risk factors for urethral stricture and/or bladder neck contracture after monopolar transurethral resection of the prostate for benign prostatic hyperplasia. Urologia. 2018;85(4):150-157. DOI: 10.1177/0391560318758195
12. Reich O, Gratzke C, Bachmann A, Seitz M, Schlenker B, Hermanek P, Lack N, Stief CG; Urology Section of the Bavarian Working Group for Quality Assurance. Morbidity, mortality and early outcome of transurethral resection of the prostate: a prospective multicenter evaluation of 10,654 patients. J Urol. 2008;180(1):246-249. DOI: 10.1016/j.juro.2008.03.058
13. Abbosov S.A., Sorokin N.I., Kadrev A.V., Shomarufov A.B., Nesterova O.Y., Akilov F.A., Kamalov A.A. Predictors of bladder neck contracture after transurethral procedure on the prostate. Urologiia. 2021;(5):73-77. (In Russian).
14. Barbalias D, Lappas G, Ravazoula P, Liourdi D, Kyriazis I, Liatsikos E, Kallidonis P. Evaluation of the Distribution of Paclitaxel After Application of a Paclitaxel-Coated Balloon in the Rabbit Urethra. J Endourol. 2018;32(5):381-386. DOI: 10.1089/end.2017.0935
15. Reva I.A., Zhivov A.V., Bernikov A.N., Pushkar’ D.Yu. Risk factors and correction methods for postoperative vesicourethral anastomotic strictures: literature review. Cancer Urology. 2017;13(2):104-112. (In Russian).
16. Favre GA, Alfieri AG, Gil Villa SA, Tobia I, Giudice CR. Bulbomembranous Urethral Strictures Repair After Surgical Treatment of Benign Prostatic Hyperplasia. Experience From a Latin American Referral Centre. Urology. 2021;147:281-286. DOI: 10.1016/j.urology.2020.08.085
17. Abbosov SA, Sorokin NI, Shomarufov AB, Kadrev AV, Ugli N, Khusniddin Z, Mukhtarov ST, Akilov FA, Kamalov AA. Bladder Neck Contracture as a Complication of Prostate Surgery. Alternative Treatment Methods and Prospects (Literature Review). Urological Science. 2022;33(2):49-55. DOI: 10.4103/UROS.UROS_127_21
18. Steenkamp JW, Heyns CF, de Kock ML. Internal urethrotomy versus dilation as treatment for male urethral strictures: a prospective, randomized comparison. J Urol. 1997;157(1):98-101. PMID: 8976225.
19. Vicente J, Salvador J, Caffaratti J. Endoscopic urethrotomy versus urethrotomy plus Nd-YAG laser in the treatment of urethral stricture. Eur Urol. 1990;18(3):166-168. DOI: 10.1159/000463901
20. Lee YH, Chiu AW, Huang JK. Comprehensive study of bladder neck contracture after transurethral resection of prostate. Urology. 2005;65(3):498-503; discussion 503. DOI: 10.1016/j.urology.2004.10.082
21. Mukhtarov Sh.T., Nasirov F.R., Bakhadirkhanov M.M., Uralova N.D., Akilov F.A., Mirkhamidov D.Kh., Shomarufov A.B., Abbosov Sh.A., Kasimov S.S. Endoscopic treatment for bulbar-membranous urethral obliteration: evaluation of the efficacy and safety. Urology Herald. 2022;10(4):79-87. (In Russian).
22. Abbosov ShA, Sorokin NI, Shomarufov AB, Kadrev AV, Mikheev KV, Fozilov AA, Nadjimitdinov YS, Ohobotov DA, Giyasov ShI, Mukhtarov ShT, Akilov FA, Kamalov AA. Assessment of the Balloon Dilation Efficiency in Bladder Neck Contracture after Transurethral Interventions on the Prostate. Urological Science. 2022;33(3):130-135. DOI: 10.4103/UROS.UROS_148_21
23. Ramchandani P, Banner MP, Berlin JW, Dannenbaum MS, Wein AJ. Vesicourethral anastomotic strictures after radical prostatectomy: efficacy of transurethral balloon dilation. Radiology. 1994;193(2):345-349. DOI: 10.1148/radiology.193.2.7972741
24. Ishii G, Naruoka T, Kasai K, Hata K, Omono H, Suzuki M, Kimura T, Egawa S. High pressure balloon dilation for vesicourethral anastomotic strictures after radical prostatectomy. BMC Urol. 2015;15:62. DOI: 10.1186/s12894-015-0059-9
25. Abbosov Sh.A., Okhobotov D.A., Sorokin N.I., Shomarufov A.B., Shaparov B.M., Nadzhimitdinov Ya.S., Mukhtarov Sh.T., Akilov F.A., Kamalov A.A. Balloon dilatation of cicatricial bladder neck contracture: evaluation of the efficacy after transurethral prostate interventions (preliminary results). Urology Herald. 2021;9(1):5-13. (In Russian).
26. Vyas JB, Ganpule AP, Muthu V, Sabnis RB, Desai MR. Balloon dilatation for male urethral strictures “revisited”. Urol Ann. 2013;5(4):245-248. DOI: 10.4103/0974-7796.120296
27. Xie TP, Huang XB, Xu QQ, Ye HY, Yang QY, Wang XF. [Balloon dilation by B ultrasound monitoring for treatment of urethral stricture: 5 case reports]. Beijing Da Xue Xue Bao Yi Xue Ban. 2014;46(4):657-658. (In Chinese). PMID: 25131490.
About the Authors
Sh. A. AbbosovUzbekistan
Shukhrat A. Abbosov — Cand.Sc.(Med).
Tashkent
Competing Interests:
None
A. B. Shomarufov
Uzbekistan
Azizbek B. Shomarufov - Cand.Sc.(Med).
Tashkent
Competing Interests:
None
D. R. Aminova
Uzbekistan
Dilafruz R. Aminova.
Tashkent
Competing Interests:
None
Review
For citations:
Abbosov Sh.A., Shomarufov A.B., Aminova D.R. Transurethral balloon dilation safety and efficacy in patients with recurrent bladder neck contracture after transurethral interventions. Urology Herald. 2024;12(4):5-13. https://doi.org/10.21886/2308-6424-2024-12-4-5-13













































