Scroll to:
Bilateral simultaneous partial nephrectomy
https://doi.org/10.21886/2308-6424-2024-12-3-125-130
Abstract
Introduction. Partial nephrectomy is the treatment of choice for small renal tumors. There are other indications include tumors in a solitary kidney, multiple and bilateral tumors.
Сase presentation. A 67-year-old male presented with left flank pain and lower urinary tract symptoms. Computed tomography for abdominal and pelvis showed bilateral renal masses. After doing the essential laboratory tests and investigations, he underwent bilateral open simultaneous partial nephrectomies. After two days, he was discharged with no complains. Follow-up after three months showed no recurrence and acceptable renal function.
Discussion. Partial nephrectomy is increasingly used for the management of renal masses. The preservation of renal function with reduced morbidity and equivalent oncologic outcomes led to a paradigm shift away from radical nephrectomy.
Conclusion. Bilateral partial nephrectomy is feasible with both clinical and oncological good results.
For citations:
AlTawil M. Bilateral simultaneous partial nephrectomy. Urology Herald. 2024;12(3):125-130. https://doi.org/10.21886/2308-6424-2024-12-3-125-130
Introduction
Partial nephrectomy is increasingly used for the management of renal masses. The preservation of renal function with reduced morbidity and equivalent oncologic outcomes led to a paradigm shift away from radical nephrectomy [1][2].
Nephron-sparing surgery is an attractive treatment option for multifocal tumors because of the potential for recurrence. Selected tumors, especially small, exophytic, and noninfiltrating lesions, can be excised without hilar clamping [3]. Even larger, deeper, central, or hilar tumors, which may require more substantial dissection and reconstruction, can be safely excised off-clamp with adequate experience [4]. Selective arterial clamping techniques by interrupting single or multiple arterial branches supplying the area of the tumor without causing global renal ischemia to have been described [5]. The theoretic advantages of this approach include a relatively bloodless field for tumor resection, without compromising blood flow to the entire kidney. Another alternative to hilar clamping is the compression of renal parenchyma that can be accomplished by hand compression [6].
Case presentation
A 67-year-old male presented to the clinic with left mild flank pain and lower urinary symptoms. He was diagnosed with diabetes mellitus and blood hypertension 10 years ago. Physical examination was normal with mild prostatic enlargement. Laboratory tests were: Hgb 11 mg/dl, Glucose 122 mg/dl, creatinine 1.4 mg/dl, urea 49 mg/dl, and Na 140 mEq/L, and K 5.1 mEq/L. Urinalysis showed microscopic hematuria and pyuria. Computed tomography (CT) scan for the abdominal and pelvis was obtained. CT scan showed bilateral renal masses (Fig. 1). Bilateral renal CT- guided biopsies was done and showed bilateral papillary renal cell carcinoma grade II. Bilateral open simultaneous partial nephrectomies were decided and done through bilateral subcostal approach (Fig. 2, 3). During surgery, we transferred one unit of blood. The right tumor was excised without hilar clamping (only compression of renal parenchyma). The left hilar was clamped before the left tumor was removed, and the collecting system was closed by running absorbable sutures.
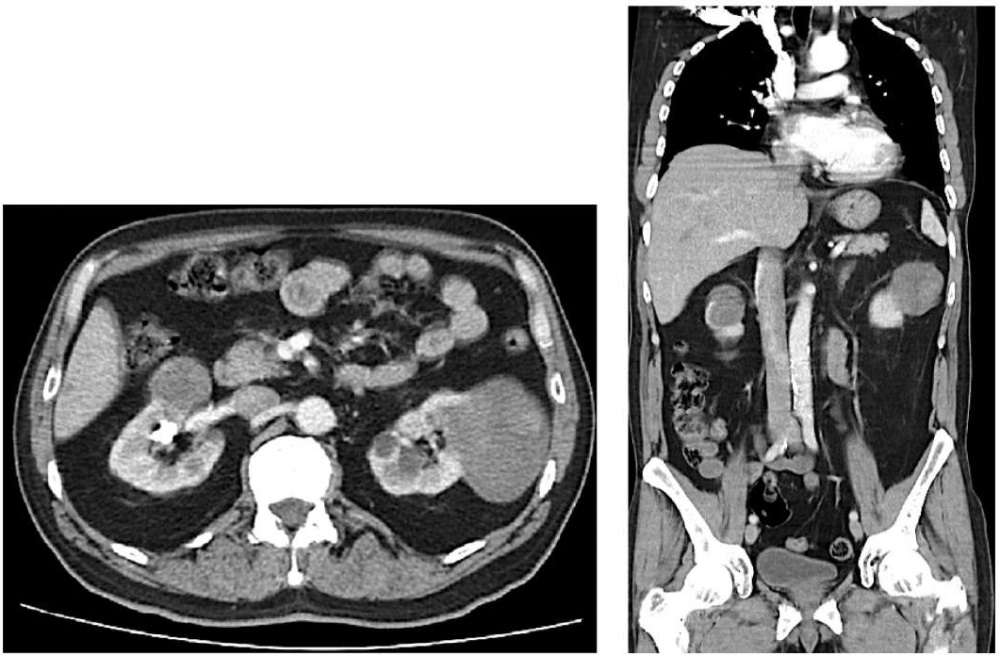
Figure 1. CT scan showing bilateral renal masses
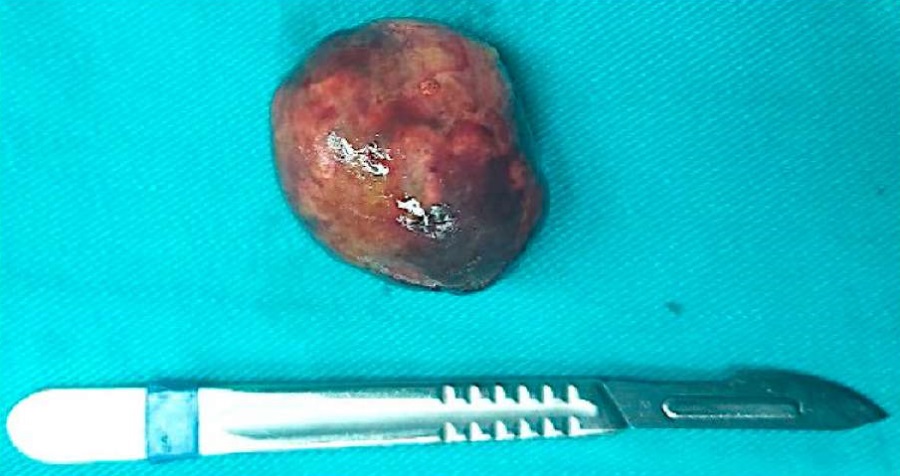
Figure 2. The right renal mass
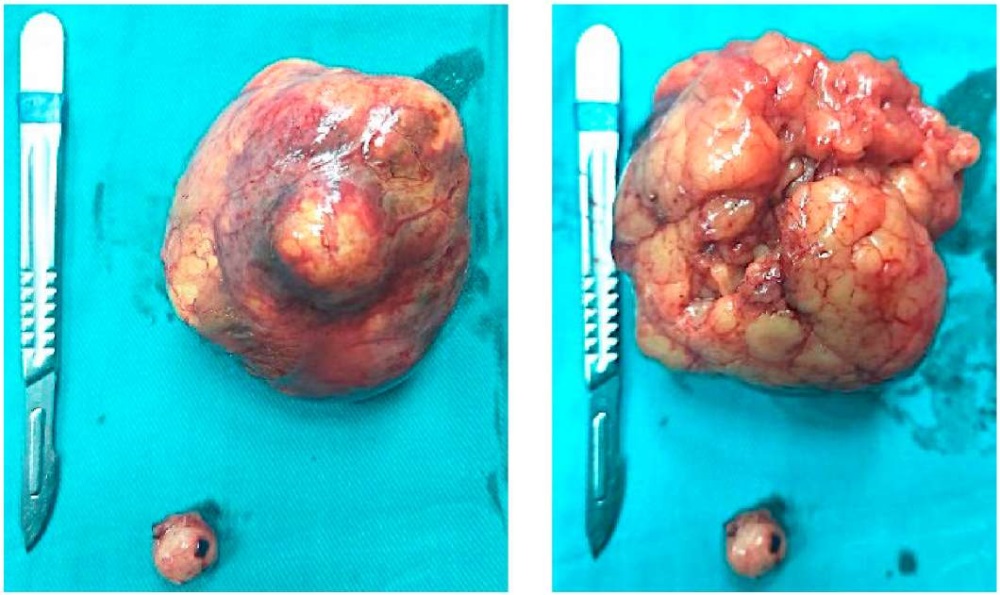
Figure 3. The left renal masses
The pathological report (Fig. 4) showed bilateral papillary renal cell carcinoma, low grade, encapsulated and measures 5 cm in right kidney and 9 cm and 1.8 cm in left kidney, both surgical margins were free.
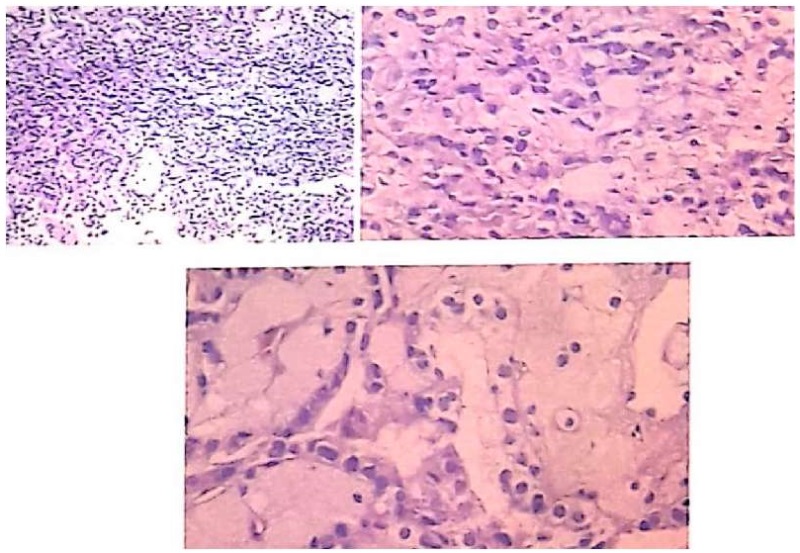
Figure 4. The pathological microscopic view
Postoperative, the patient spent two days in the hospital. Daily blood tests were with in normal limits. Follow-up after three months with laboratory and radiology work-up demonstrated full recovery and no recurrence.
Discussion
There are no randomized clinical trials comparing partial with radical nephrectomy in the management of large renal masses, retrospective studies have shown feasibility and safety of nephron-sparing surgery for large renal tumors [7].
Radical nephrectomy was associated with a nearly 30% decline in estimated glomerular filtration rate compared with only 12% in the partial nephrectomy group. A study of 133 open, 57 laparoscopic, and 95 robot-assisted partial nephrectomies for the management of pT1b renal tumors showed comparable perioperative complications, negative surgical margins, and ischemia time across all three surgical approaches [8]. Shah et al. looked at 1250 partial nephrectomies and found a 27% rate of upstaging in patients with clinical T1b compared with 4.4% in patients with clinical T1a disease. Furthermore, 33% of these recurred. Caution should be taken when applying partial nephrectomy to larger tumors [9].
Tumor complexity can be characterized using RENAL nephrometry score, which takes into consideration tumor Radius, Exophytic/endophytic appearance, Nearness to the collecting system, Anterior/posterior position, and Location relative to the polar line [10]. Anatomic complexity measured by RENAL nephrometry has been shown to correlate with risk of complications, warm ischemia time, operative time, hospital stay, estimated blood loss, and risk of recurrence after surgery [11].
Nephron-sparing surgery is an attractive treatment option for multifocal tumors because of the potential for recurrence. In a matched analysis of 33 patients undergoing partial nephrectomy for multiple tumors, resection of multiple tumors was associated with long operative time and hospitalization with comparable blood loss, complication rates, and renal functional outcomes [12]. Bilateral laparoscopic partial nephrectomies can be performed in a staged or single-setting fashion. In a study of 13 cases of bilateral renal masses, 11 (85%) were successfully treated in a single setting [13]. The authors concluded that bilateral single setting surgery is feasible and should only be performed in select cases when the primary procedure has been completed expeditiously and without complications.
Selected tumors, especially small, exophytic, and non-infiltrating lesions, can be excised without hilar clamping [3]. Even larger, deeper, central, or hilar tumors, which may require more substantial dissection and reconstruction, can be safely excised off-clamp with adequate experience [4][5]. A meta-analysis of 10 studies including 728 off-clamp and 1267 on-clamp partial nephrectomies found that off-clamp surgery had a higher blood transfusion rate but lower overall postoperative complication rate, lower positive margin rate, and better preservation of renal function than the on-clamp approach [14].
A study including only partial nephrectomy in solitary kidneys found the off-clamp technique to be associated with improved estimated GFR in the early and late postoperative periods [15].
Selective arterial clamping techniques by interrupting single or multiple arterial branches supplying the area of the tumor without causing global renal ischemia to have been described [5]. The theoretic advantages of this approach include a relatively bloodless field for tumor resection, without compromising blood flow to the entire kidney. A retrospective study of 121 partial nephrectomies comparing selective arterial clamping with hilar clamping found selective clamping to be associated with improved postoperative renal function, longer operative times, higher transfusion rates, and comparable perioperative complication rates and length of hospital stay [16].
Another alternative to hilar clamping is the compression of renal parenchyma that can be accomplished by hand compression. Reports using these techniques have demonstrated their feasibility and safety in selected cases, especially in cases of peripherally located tumors [6][17].
The feasibility, safety, and effectiveness of minimally invasive partial nephrectomy have been demonstrated by several authors [2][18] Studies comparing laparoscopic and open partial nephrectomy with radical nephrectomy suggest that nephron-sparing surgery is associated with equivalent oncologic outcomes in properly selected patients and improved overall survival, likely resulting from reduced rates of renal insufficiency and cardiovascular morbidity [19].
In multivariate analysis, predictors of metastasis included larger tumor size, absolute indication, and comorbidity but not surgical approach. The authors concluded that laparoscopic and open partial nephrectomy provide equivalent long-term overall and recurrence-free survival for pT1 tumors.
Multiple authors compared robot-assisted partial nephrectomy with open nephrectomy showing similar benefits of the robot-assisted approach, including less estimated blood loss, shorter hospital stay, and lower complications rates with comparable warm ischemia times and positive margin rates [20]. Two meta-analyses, one including 8 retrospective studies and 3418 surgeries and another including 16 studies and 3024 surgeries, comparing robot assisted to open partial nephrectomy demonstrated that the robot-assisted approach was associated with a lower rate of perioperative complications, less estimated blood loss, and shorter length of hospital stay with comparable conversion to radical nephrectomy, warm ischemia time, estimated GFR changes, margin status, and overall cost [21][22].
Conclusion
Bilateral partial nephrectomy is feasible with both good clinical and oncological results.
References
1. Gill IS, Kavoussi LR, Lane BR, Blute ML, Babineau D, Colombo JR Jr, Frank I, Permpongkosol S, Weight CJ, Kaouk JH, Kattan MW, Novick AC. Comparison of 1,800 laparoscopic and open partial nephrectomies for single renal tumors. J Urol. 2007;178(1):41-46. DOI: 10.1016/j.juro.2007.03.038
2. Lane BR, Gill IS. 7-year oncological outcomes after laparoscopic and open partial nephrectomy. J Urol. 2010;183(2):473-479. DOI: 10.1016/j.juro.2009.10.023
3. Novak R, Mulligan D, Abaza R. Robotic partial nephrectomy without renal ischemia.. 2012;79(6):1296-1301. DOI: Urology10.1016/j.urology.2012.01.065
4. Kreshover JE, Kavoussi LR, Richstone L. Hilar clamping versus off-clamp laparoscopic partial nephrectomy for T1b tumors. Curr Opin Urol. 2013;23(5):399-402. DOI: 10.1097/MOU.0b013e3283632115
5. Patil MB, Gill IS. Zero-ischaemia robotic and laparoscopic partial nephrectomy (PN). BJU Int. 2011;108(5):780-792. DOI: 10.1111/j.1464-410X.2011.10564.x
6. Simon J, Bartsch G Jr, Finter F, Hautmann R, de Petriconi R. Laparoscopic partial nephrectomy with selective control of the renal parenchyma: initial experience with a novel laparoscopic clamp. BJU Int. 2009;103(6):805-808. DOI: 10.1111/j.1464-410X.2008.08112.x
7. Simmons MN, Weight CJ, Gill IS. Laparoscopic radical versus partial nephrectomy for tumors >4 cm: intermediate-term oncologic and functional outcomes. Urology. 2009;73(5):1077-1082. DOI: 10.1016/j.urology.2008.11.059
8. Porpiglia F, Mari A, Bertolo R, Antonelli A, Bianchi G, Fidanza F, Fiori C, Furlan M, Morgia G, Novara G, Rocco B, Rovereto B, Serni S, Simeone C, Carini M, Minervini A. Partial Nephrectomy in Clinical T1b Renal Tumors: Multicenter Comparative Study of Open, Laparoscopic and Robot-assisted Approach (the RECORd Project). Urology. 2016;89:45-51. DOI: 10.1016/j.urology.2015.08.049
9. Shah PH, George AK, Moreira DM, Alom M, Okhunov Z, Salami S, Waingankar N, Schwartz MJ, Vira MA, Richstone L, Kavoussi LR. To clamp or not to clamp? Long-term functional outcomes for elective off-clamp laparoscopic partial nephrectomy. BJU Int. 2016;117(2):293-299. DOI: 10.1111/bju.13309
10. Kutikov A, Uzzo RG. The R.E.N.A.L. nephrometry score: a comprehensive standardized system for quantitating renal tumor size, location and depth. J Urol. 2009;182(3):844-853. DOI: 10.1016/j.juro.2009.05.035
11. Watts KL, Ghosh P, Stein S, Ghavamian R. Value of Nephrometry Score Constituents on Perioperative Outcomes and Split Renal Function in Patients Undergoing Minimally Invasive Partial Nephrectomy. Urology. 2017;99:112-117. DOI: 10.1016/j.urology.2016.01.046
12. Abreu AL, Berger AK, Aron M, Ukimura O, Stein RJ, Gill IS, Desai MM. Minimally invasive partial nephrectomy for single versus multiple renal tumors. J Urol. 2013;189(2):462-467. DOI: 10.1016/j.juro.2012.09.039
13. Reisiger K, Tran V, Figenshau RS, Andriole GL, Landman J. Single-setting bilateral laparoscopic renal surgery: assessment of single-stage procedure. Urology. 2005;65(5):892-897; discussion 897. DOI: 10.1016/j.urology.2004.11.055
14. Liu W, Li Y, Chen M, Gu L, Tong S, Lei Y, Qi L. Off-clamp versus complete hilar control partial nephrectomy for renal cell carcinoma: a systematic review and meta-analysis. J Endourol. 2014;28(5):567-576. DOI: 10.1089/end.2013.0562
15. Wszolek MF, Kenney PA, Lee Y, Libertino JA. Comparison of hilar clamping and non-hilar clamping partial nephrectomy for tumours involving a solitary kidney. BJU Int. 2011;107(12):1886-1892. DOI: 10.1111/j.1464-410X.2010.09713.x
16. Desai MM, de Castro Abreu AL, Leslie S, Cai J, Huang EY, Lewandowski PM, Lee D, Dharmaraja A, Berger AK, Goh A, Ukimura O, Aron M, Gill IS. Robotic partial nephrectomy with superselective versus main artery clamping: a retrospective comparison. Eur Urol. 2014;66(4):713-719. DOI: 10.1016/j.eururo.2014.01.017
17. Verhoest G, Manunta A, Bensalah K, Vincendeau S, Rioux-Leclercq N, Guillé F, Patard JJ. Laparoscopic partial nephrectomy with clamping of the renal parenchyma: initial experience. Eur Urol. 2007;52(5):1340-1346. DOI: 10.1016/j.eururo.2007.04.072
18. Permpongkosol S, Bagga HS, Romero FR, Sroka M, Jarrett TW, Kavoussi LR. Laparoscopic versus open partial nephrectomy for the treatment of pathological T1N0M0 renal cell carcinoma: a 5-year survival rate. J Urol. 2006;176(5):1984-1988; discussion 1988-1989. DOI: 10.1016/j.juro.2006.07.033
19. Thompson RH, Boorjian SA, Lohse CM, Leibovich BC, Kwon ED, Cheville JC, Blute ML. Radical nephrectomy for pT1a renal masses may be associated with decreased overall survival compared with partial nephrectomy. J Urol. 2008;179(2):468-471; discussion 472-473. DOI: 10.1016/j.juro.2007.09.077
20. Wang Y, Shao J, Ma X, Du Q, Gong H, Zhang X. Robotic and open partial nephrectomy for complex renal tumors: a matched-pair comparison with a long-term follow-up. World J Urol. 2017;35(1):73-80. DOI: 10.1007/s00345-016-1849-8
21. Shen Z, Xie L, Xie W, Hu H, Chen T, Xing C, Liu X, Xu H, Zhang Y, Wu Z, Tian D, Wu C. The comparison of perioperative outcomes of robot-assisted and open partial nephrectomy: a systematic review and meta-analysis. World J Surg Oncol. 2016;14(1):220. DOI: 10.1186/s12957-016-0971-9
22. Wu Z, Li M, Liu B, Cai C, Ye H, Lv C, Yang Q, Sheng J, Song S, Qu L, Xiao L, Sun Y, Wang L. Robotic versus open partial nephrectomy: a systematic review and meta-analysis. PLoS One. 2014;9(4):e94878. DOI: 10.1371/journal.pone.0094878
About the Author
M. AlTawilSyrian Arab Republic
Muhamad AlTawil — M.D., Ph.D.
Faculty of Medicine
Damascus
Review
For citations:
AlTawil M. Bilateral simultaneous partial nephrectomy. Urology Herald. 2024;12(3):125-130. https://doi.org/10.21886/2308-6424-2024-12-3-125-130













































