Scroll to:
Сomparison of biomechanical properties of non-absorbable and partially absorbable mesh implants used in surgery for urinary incontinence and genital prolapse: experimental study
https://doi.org/10.21886/2308-6424-2023-11-1-116-124
Abstract
Introduction. The amount of non-absorbable synthetic material used in the surgical treatment of pelvic organ prolapse and stress urinary incontinence has been shown to directly correlate with the risks of mesh-associated complications. Previously, we developed a partially absorbable implant. Currently, there are insufficient data on the use of partially absorbable implants in female pelvic floor reconstruction, which requires comparative biomechanical and pathomorphological studies.
Objective. To compare the biomechanical properties of a new generation partially absorbable implants and nonabsorbable polypropylene mesh implants during animal model.
Materials & methods. Thirty-nine rabbits weighing 3200 ± 250 g were randomised into three groups depending on the implanted endoprosthesis: group 1 (n = 15) — “Axilen” implant (polydioxanone 98%, polypropylene 2%), group 2 (n = 15) — “Axilen Rapid” implant (polyglycapron 98%, polypropylene 2%), group 3 (n = 9) — “Urosling 1” implant. After implantation, rabbits of all 3 groups were divided into 3 subgroups according to the withdrawal period from the experiment: 14 days, 60 days, and 180 days. The biomaterial obtained was subjected to two studies: evaluation of the macroscopic view of the explanted mesh endoprosthesis with the formed capsule and the surrounding tissues, study of the biomechanical properties of the formed connective tissue capsule with the implant.
Results. According to macroscopic evaluation, there was a less significant tissue reaction to partially absorbed implants. A comparative analysis of biomechanical indices revealed no statistically significant difference in rupture elongation at all follow-up periods among the presented groups. Tensile strength, at 60 and 180 days, was not statistically different between the groups described. At 14 days, there was a statistically significant difference in tensile strength between groups 1 and 3 (p = 0.003).
Conclusion. During biomechanical animal experiments, the connective tissue capsule formed on the partially absorbable implant was not inferior to the similar parameter of the non-absorbable sample in its tensile strength, which explains a great potential for the use of partially absorbable implants in reconstructive surgery of pelvic organ prolapse and stress urinary incontinence.
For citations:
Shkarupa D.D., Shakhaliev R.A., Shulgin A.S., Filipenko T.S., Kubin N.D., Labetov I.A., Suchkov D.A. Сomparison of biomechanical properties of non-absorbable and partially absorbable mesh implants used in surgery for urinary incontinence and genital prolapse: experimental study. Urology Herald. 2023;11(1):116-124. (In Russ.) https://doi.org/10.21886/2308-6424-2023-11-1-116-124
Introduction
The use of mesh grafts plays an important role in the surgical treatment of pelvic organ prolapse (POP) and stress urinary incontinence (SUI) [1][2]. In turn, the most common synthetic material for manufacturing mesh grafts is polypropylene [3]. The application of permanent mesh grafts is associated with a relatively high risk of mesh-associated complications that significantly reduce patients' quality of life. Vaginal wall erosion and chronic pelvic pain are the most common [4]. It is proven that the amount of non-absorbable synthetic material used directly affects the risk of the complications mentioned above [5]. Moreover, some countries banned the use of transvaginal mesh implants for surgical reconstruction of the pelvic floor due to an active discussion around reports of complications of this type of surgery [6]. Thus, there is a clear need to develop a new generation of synthetic grafts with a low content of non-resorbable material but retaining all the advantages of mesh implants. Previously, the authors of the present study evaluated the mechanical characteristics of a partially resorbable implant in vitro [7]. The experimental results showed that the strength of this type of grafts at any time of resorption was sufficient according to the potential load on the graft in the soft tissues of the human body.
Currently, there are insufficient data on the use of partially resorbable implants in the surgical treatment of POP and SUI, which requires comparative biomechanical and pathomorphological studies.
The study aimed to compare of biomechanical properties of a new generation of partially resorbable grafts and non-resorbable polypropylene mesh grafts on a rabbit model.
Materials and Methods
The study was performed in accordance with the ethical standards for the treatment of animals adopted by the European Convention for the Protection of Vertebrate Animals used for Experimental and other Scientific Purposes (CETS 123), the Federation of European Laboratory Animal Science Associations (FELASA), and the International Council for Laboratory Animal Science (ICLAS). The study was conducted on 39 male Chinchilla rabbits with an average weight of 3200 ± 250 g. Laboratory animals were obtained and housed in the vivarium of the Northwestern State Medical University named after I.I. Mechnikov. Then, they were randomized into 3 groups according to the implanted material: 15 rabbits (group 1) were implanted with a partially resorbable ligature delivery system “Axilen”© graft (OOO Lintex, St. Petersburg, Russia) consisting of 98% polydioxanone and 2% polypropylene, 15 rabbits (group 2) were implanted with a semi-resorbable ligature delivery system “Axilen Rapid”© graft (OOO Lintex, St. Petersburg, Russia) consisting of 98% polyglycapron and 2% polypropylene, and a non-absorbable polypropylene mesh graft “Urosling 1”© (OOO Lintex, St. Petersburg, Russia) was implanted in 9 rabbits (group 3). The resorption period of polydiaxanone was 4–6 months, and that of polyglycapron was 1–2 months.
- The size of the mesh grafts was standardised to 10.0 × 1.5 cm for all endoprostheses. After implantation, rabbits from all 3 groups were randomly divided into 3 equal subgroups according to the withdrawal period from the experiment: 14 days, 60 days, and 180 days.
- When the rabbit was removed from the experiment, the biomaterial underwent 2 examinations:
- Evaluation of the macroscopic condition of the explanted mesh graft with the capsule formed and surrounding tissues;
- Study of the biomechanical properties of the connective tissue capsule formed with the graft.
Description of the surgical intervention. The surgical technique was standardized for all 3 groups of rabbits. After induction of general anaesthesia (2 preparations), the abdominal surface of the rabbit was shaved, the surgical field was treated twice with antiseptic and all surgical manipulations were performed using sterile instruments. On the skin of the anterior abdominal wall, two transverse parallel incisions were made symmetrically to the central line, 2 cm long, 11 cm apart. Further, subcutaneous dissection of the tissues in the layer above the abdominal muscles without entering the abdominal cavity was performed, the mesh graft was introduced subcutaneously through the guide and fixed to the anterior abdominal wall muscles with a thread with the formation of two loop sutures from each end of the mesh graft. After that, the skin was sutured with loop sutures. Fixation of the mesh graft and suturing of the skin were performed using USP 3-0 monofilament polypropylene thread.
The animals were withdrawn from the experiment on the appropriate term after implantation. A 12 × 3 cm section of the abdominal wall was dissected through all layers up to the anterior peritoneal layer, including the previously installed endoprosthesis.
The biomaterial obtained was divided into two parts:
- 1/10 of the implanted graft length with the surrounding tissues was placed in a container with formalin for a morphological study;
- the remaining material (9/10 of the implanted graft length) was subjected to additional dissection to separate the implant with the formed connective tissue capsule for a study of biomechanical properties. The material was placed in a container with a 0.9% NaCl saline solution.
Biomechanical Analysis. The material for biomechanical analysis was examined on the day of explantation at the technical laboratory of OOO Lintex. Biomechanical properties were assessed on an INSTRON 5900 series universal electromechanical testing machine (Instron, Illinois Tool Works Inc., Glenview, IL, USA). The samples were fixed in the clamps of the tensile machine with the edges prestitched with ligatures to prevent slipping. The distance between the clamps was 3 to 5 cm. Uniaxial tensile strength (N/cm) and rupture elongation (%) were recorded.
Statistical analysis. Quantitative characteristics were described as the mean ± standard deviation (mean-square deviation). Absolute values (n) and percentage (%) were used to describe qualitative characteristics.
One-factor analysis of variance (ANOVA) was used to compare the groups. Tukey's HSD test was used for pairwise comparison between the groups.
The two-sided significance level for all tests was set at p < 0.05. All calculations were performed using R version 4.1.3 (The R Foundation for Statistical Computing, Vienna, Austria) in compliance with reproducibility criteria.
Results
Macroscopic analysis. All 39 rabbits were withdrawn from the experiment within the specified timeframe. There was no death or significant decrease in the body weight of rabbits in any of the studied groups. Examination revealed no abscesses or purulent necrotic changes in the implantation area. Table 1 shows pictures of rabbits withdrawn from the experiment at the corresponding terms with the dissected implant site.
Table 1. Macroscopic analysis
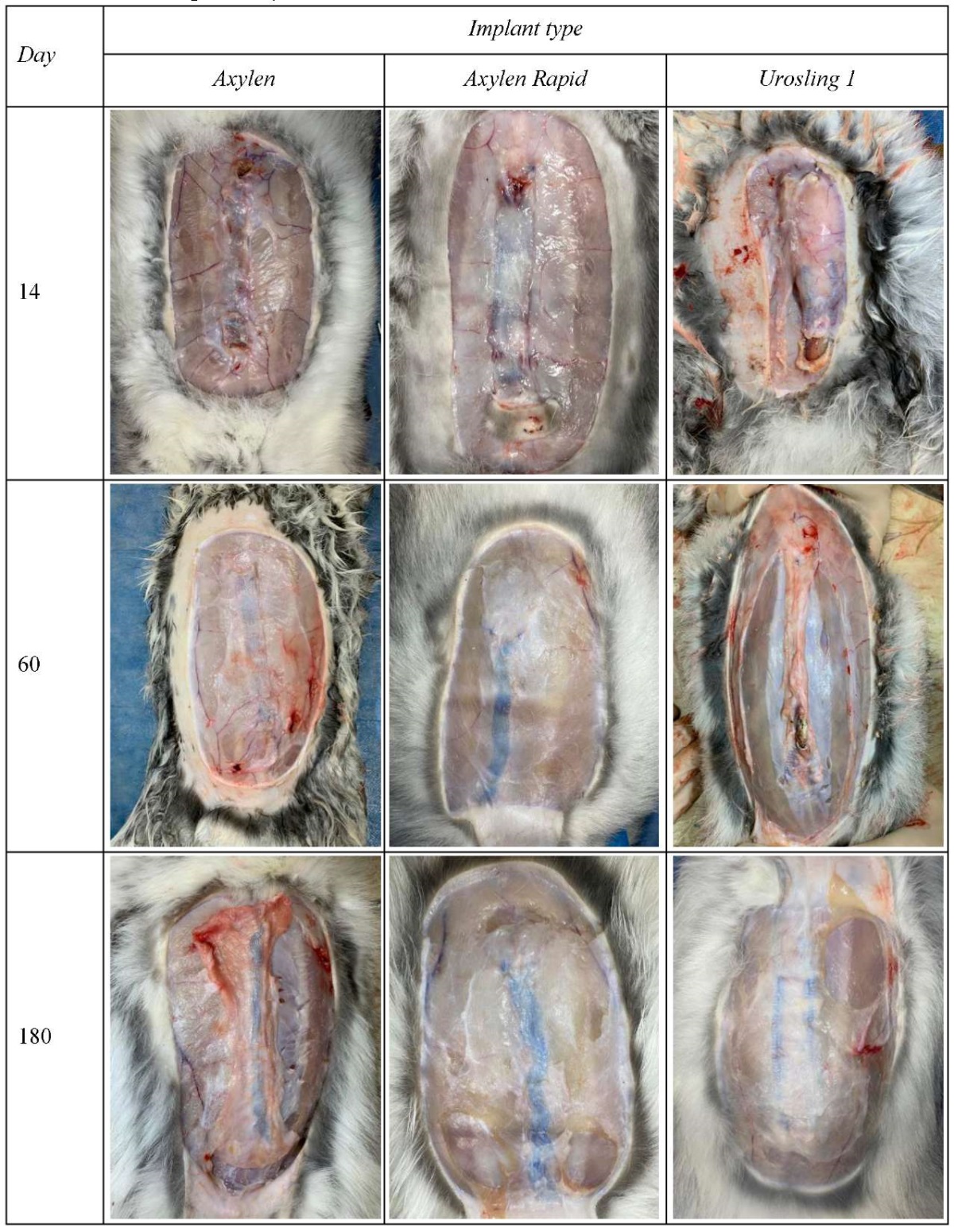
On day 14, in group 3, two out of three animals showed pronounced exudation around the capsule formed around the graft; the mesh graft was not deformed. In the same period, in groups 1 and 2, these signs were absent and only capsule formation around the graft was observed. Furthermore, in group 2, the initial stages of resorption of the resorbable component were visualised. At the same time, the non-absorbable sutures lay flat and the graft was not deformed.
On day 60, in group 3, there was a small amount of exudate in the area of the formed graft capsule. The capsule was more rigid compared to groups 1 and 2. All three rabbits showed moderate lateral corrugation of the mesh graft without shrinkage along its length. In group 2, a soft connective tissue capsule was formed, and the resorption of the resorbable component was complete. The polypropylene thread chains were located symmetrically inside the formed connective tissue capsule, with insignificant deformation, without shrinkage along the length. There were no macroscopic signs of inflammation, but a small amount of transparent exudate was detected. The resorption of the resorbable component continued in group 1. The graft was not deformed and was symmetrically located within the soft connective tissue capsule formed with an insignificant amount of transparent exudate.
On day 180, in group 3, all rabbits had almost no exudate in the area of the dense connective tissue capsule. There was also moderate lateral corrugation of the mesh graft in all 3 rabbits without shrinkage in length, as in rabbits after 60 days of the experiment. The formation of a denser capsule was detected in group 2 compared to 60 days; no change was detected in the other indices evaluated. Group 1 also showed a denser capsule than at 60 days. The resorption process of the resorbable component was completed; the chains of polypropylene threads were symmetrically laid with a slight deformation in the lateral direction without changing the original graft length (Fig.).
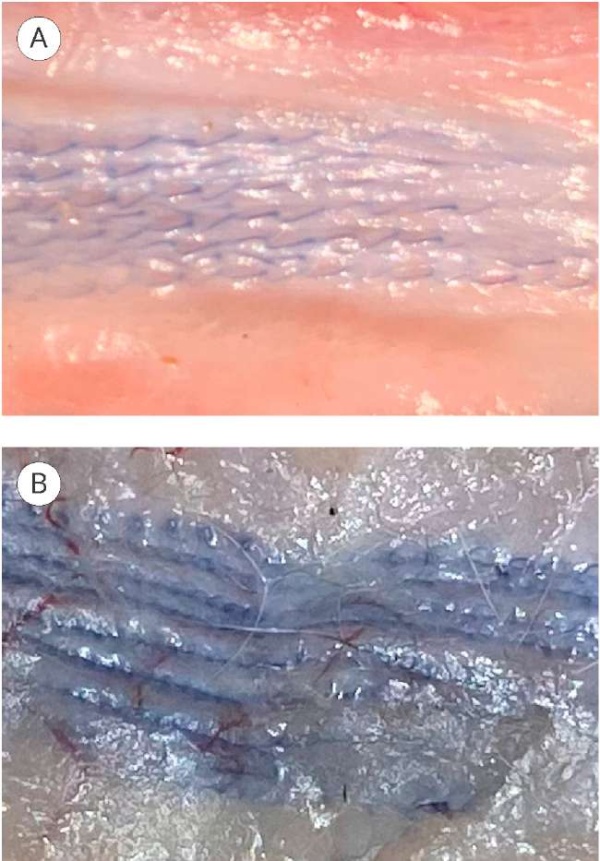
Figure. Macroscopic photo of polypropylene sutures at 180 days of implantation: А — Axilen; В — Axilen Rapid
Table 2 shows the macroscopic characteristics of all types of explanted material at different terms of the withdrawal of rabbits from the experiment.
Table 2. Macroscopic characteristics of all explants types at different periods of animal withdrawal from the experiment
|
Sign |
Axilen |
Axilen Rapid |
Urosling 1 |
||||||
|
withdrawal period, day |
|||||||||
|
14 |
60 |
180 |
14 |
60 |
180 |
14 |
60 |
180 |
|
|
Exudation |
+ |
+ |
+ |
+ |
+ |
+ |
+++ |
++ |
+ |
|
Scar density |
+ |
+ |
++ |
+ |
+ |
++ |
++ |
+++ |
+++ |
|
Implant deformation |
– |
– |
+ |
– |
+ |
+ |
– |
++ |
++ |
|
Implant absorption |
– |
++ |
+++ |
++ |
+++ |
+++ |
– |
– |
– |
Note:
– — no sign;
+ — weak sign;
++ — moderate sign;
+++ — pronounced sign
Biomechanical analysis. A comparative analysis of the biomechanical indices (Tab. 3) did not reveal any statistically significant differences in rupture elongation in all follow-up periods among the studied groups. Tensile strength (Tab. 4) after 60 and 180 days was not statistically different between the studied groups. After 14 days, there was a statistically significant difference in the tensile strength between groups 1 and 3 (p = 0.003).
Table 3. Results of comparative analysis of rupture elongation in different follow-up periods
|
Period, day |
Axilen |
Axilen Rapid |
Urosling 1 |
p |
|
14 |
86 ± 10 |
83 ± 26 |
65 ± 23 |
0.400 |
|
60 |
28 ± 7 |
36 ± 30 |
73 ± 48 |
0.150 |
|
180 |
31 ± 12 |
32 ± 13 |
28 ± 3 |
0.900 |
Note. Rupture elongation is indicated in %
Table 4. Results of comparative analysis of breaking in at different follow-up periods
|
Period, day |
Axilen |
Axilen Rapid |
Urosling 1 |
p |
|
14 |
59 ± 7* |
72 ± 9 |
87 ± 10* |
0.004 |
|
60 |
81 ± 18 |
66 ± 12 |
77 ± 50 |
0.700 |
|
180 |
130 ± 27 |
168 ± 86 |
143 ± 61 |
0.600 |
Notes. Breaking load in N/cm; * — statistically significant differences by Tukey’s HSD test for pairwise comparisons
Discussion
The results of this in vivo experiment showed that there was no significant difference in the tensile strength between partially resorbable and non-resorbable polypropylene grafts after 60 and 180 days, even though the amount of permanent material was not comparable at these time points. This fact suggests that the durability is provided not only by several non-twisted polypropylene strands but also by the formed graft capsule. The results of macroscopic analysis demonstrated a more pronounced exudative reaction of the rabbit body in response to more permanent material, which is comparable to the results of earlier studies.
Thus, O'Shaughnessy et al. in their study compared the biomechanical parameters of a fully resorbable poly-4-hydroxybutyrate graft and a polypropylene mesh graft in an experiment on rabbits. The results of the study did not reveal any statistically significant differences in scar strength between grafts [8]. An unquestionable disadvantage of a fully resorbable implant is the absence of a substrate to maintain tissue fibrosis. There is not enough data on the study of resorbable grafts in pelvic floor surgery for POP and SUI. However, such grafts became widespread in hernia surgery. For example, clinical studies of fully resorbable hernia grafts showed that, despite a significant reduction in the risk of chronic pain after 3 years of follow-up, the recurrence rate reached 37.5 to 44.0%, which is certainly high for this type of surgery [9][10]. In a study by Bellónet et al., the authors compared the biomechanical characteristics of partially resorbable Vypro II, Ultrapro (Ethicon Inc., Johnson & Johnson Company, Cincinnati, OH, USA) and polypropylene grafts in a rabbit experiment. The results of the experiment also showed no significant differences in tensile strength indices [11]. However, the polypropylene threads of the Vypro II and Ultrapro grafts have a mesh structure and promote specific complications in mesh grafts. Thus, according to studies, the percentage of extrusion of Vypro II mesh into the vaginal cavity was 14%, and the development of mesh-associated pelvic pain requiring removal was 18% [12][13].
The present experiment is the first study of its kind on this type of resorbable graft. A larger sample and a longer follow-up period are probably required to reveal a significant difference in the biomechanical properties of the grafts presented in this study.
Conclusion
A biomechanical experiment in rabbits showed that the connective tissue capsule formed on the partially resorbable implant was not inferior to that of the non-resorbable specimen by the tensile strength parameter.
The small amount of permanent material in tissues and the absence of a mesh form factor in the long-term postoperative period reduce the risk of specific complications typical for polypropylene mesh grafts. This fact leads to great potential for the use of partially resorbable grafts in reconstructive surgery for POP and SUI. More comparative morphological studies are required to evaluate the response of the in vivo tissue to the implantation of resorbable grafts and clinical studies on the use of this type of grafts.
References
1. Adamyan L. V., Andreeva E.N., Artymuk N.V., Belokrinickaya E.V., Bezhenar' V.F., Gvozdev M.YU., Kasyan G.R., Kiselev S.I., Malyshkina A.I., Popov A.A., Pushkar' D.YU., Filippov O.S. Vypadenie zhenskih polovyh organov. Klinicheskie rekomendacii. 2021. (In Russian). https://cr.minzdrav.gov.ru/schema/647_1?ysclid=lapspmlikv206647769
2. Kasyan G.R., Gazimiev M.A., Gadzhieva Z.K., Zajcev A.V., Tkacheva O.N., Krivoborodov G.G., Kotovskaya YU.V., Mil’to A.S., Ostapenko V.S., Runihina N.K., Frolova E.V., Sharashkina N.V. Nederzhanie mochi. Klinicheskie rekomendacii. 2020. (In Russian). URL: https://cr.minzdrav.gov.ru/schema/8_1.
3. Ugianskiene A, Davila GW, Su TH; FIGO Urogynecology and Pelvic Floor Committee. FIGO review of statements on use of synthetic mesh for pelvic organ prolapse and stress urinary incontinence. Int J Gynaecol Obstet. 2019;147(2):147-155. DOI: 10.1002/ijgo.12932
4. Maher C, Feiner B, Baessler K, Christmann-Schmid C, Haya N, Marjoribanks J. Transvaginal mesh or grafts compared with native tissue repair for vaginal prolapse. Cochrane Database Syst Rev. 2016;2(2):CD012079. DOI: 10.1002/14651858.CD012079
5. Liang R, Knight K, Abramowitch S, Moalli PA. Exploring the basic science of prolapse meshes. Curr Opin Obstet Gynecol. 2016;28(5):413-9. DOI: 10.1097/GCO.0000000000000313
6. Shakhaliev R.A., Shulgin A.S., Kubin N.D., Kuzmina I.N., Suchkov D.A., Shkarupa D.D. Current status of transvaginal mesh implants use in the surgical treatment of stress urinary incontinence and pelvic prolapse. Gynecology. 2022;24(3):174-180. (In Russian). DOI: 10.26442/20795696.2022.3.201423
7. Shkarupa D.D., Shakhaliev R.A., Shulgin A.S., Filipenko T.S., Kubin N.D., Suchkov D.A., Shkarupa O.A. New-generation synthetic implants for the surgical correction of pelvic organ prolapse and stress urinary incontinence: design and testing. Urology Herald. 2022;10(4):109-119. (In Russian). DOI: 10.21886/2308-6424-2022-10-4-109-119
8. O’Shaughnessy D, Grande D, El-Neemany D, Sajjan S, Pillalamarri N, Shalom D, Winkler H. Evaluation of the histological and biomechanical properties of poly-4- hydroxybutyrate scaffold for pelvic organ prolapse, compared with polypropylene mesh in a rabbit model. Int Urogynecol J. 2022;33(8):2213-2220. DOI: 10.1007/s00192-021-04851-6
9. Symeonidis D, Efthimiou M, Koukoulis G, Athanasiou E, Mamaloudis I, Tzovaras G. Open inguinal hernia repair with the use of polyglycolic acid/trimethylene carbonate absorbable mesh: a critical update of the long-term results. Hernia. 2013;17(1):85-7. DOI: 10.1007/s10029-012-1016-0
10. Ruiz-Jasbon F, Norrby J, Ivarsson ML, Björck S. Inguinal hernia repair using a synthetic long-term resorbable mesh: results from a 3-year prospective safety and performance study. Hernia. 2014;18(5):723-30. DOI: 10.1007/s10029-014-1249-1
11. Bellón JM, Rodríguez M, García-Honduvilla N, Pascual G, Buján J. Partially absorbable meshes for hernia repair offer advantages over nonabsorbable meshes. Am J Surg. 2007;194(1):68-74. DOI: 10.1016/j.amjsurg.2006.11.016
12. Maher C, Baessler K, Glazener CM, Adams EJ, Hagen S. Surgical management of pelvic organ prolapse in women: a short version Cochrane review. Neurourol Urodyn. 2008;27(1):3-12. DOI: 10.1002/nau.20542
13. El Haddad R, Martan A, Masata J, Svabík K, Koleska T. Dlouhodobé lécebné výsledky vysoké zadní plastiky s plikací levátorů s pouzitím sít’ky Vypro II [Long-term review on posterior colporrhaphy with levator ani muscles plication and incorporating a Vypro II mesh]. Ceska Gynekol. 2009;74(4):282-5. (In Czech). PMID: 20564983
About the Authors
D. D. ShkarupaRussian Federation
Dmitry D. Shkarupa — M.D., Dr.Sc.(Med); Director, Pirogov Clinic of Advanced Medical Technologies (SPSU Hospital), St. Petersburg State University,
St. Petersburg
R. A. Shakhaliev
Russian Federation
Rustam A. Shakhaliev — M.D.; Gynecologist, Urology Division, Pirogov Clinic of Advanced Medical Technologies (SPSU Hospital),
St. Petersburg
A. S. Shulgin
Russian Federation
Andrei S. Shulgin — M.D., Сand.Sc. (Med); Deputy Director for Clinical, Chief Medical Officer, Pirogov Clinic of Advanced Medical Technologies (SPSU Hospital),
St. Petersburg
T. S. Filipenko
Russian Federation
Tatiana S. Filipenko — Сand.Sc.(Tech); Chief Technologist,
St. Petersburg
N. D. Kubin
Russian Federation
Nikita D. Kubin — M.D., Dr.Sc.(Med); Urologist, Urology Division, Pirogov Clinic of Advanced Medical Technologies (SPSU Hospital),
St. Petersburg
I. A. Labetov
Russian Federation
Ivan A. Labetov — M.D.; Urologist, Expert Urogynecology and Neurourology Division, Pirogov Clinic of Advanced Medical Technologies (SPSU Hospital),
St. Petersburg
D. A. Suchkov
Russian Federation
Denis A. Suchkov — M.D.; Urologist, Urology Division, Pirogov Clinic of Advanced Medical Technologies (SPSU Hospital),
St. Petersburg
Review
For citations:
Shkarupa D.D., Shakhaliev R.A., Shulgin A.S., Filipenko T.S., Kubin N.D., Labetov I.A., Suchkov D.A. Сomparison of biomechanical properties of non-absorbable and partially absorbable mesh implants used in surgery for urinary incontinence and genital prolapse: experimental study. Urology Herald. 2023;11(1):116-124. (In Russ.) https://doi.org/10.21886/2308-6424-2023-11-1-116-124













































