Scroll to:
Novel patented minimally invasive technique for surgical treatment of varicocele: technique overview
https://doi.org/10.21886/2308-6424-2023-11-1-52-58
Abstract
Introduction. Many methods have been proposed for the surgical treatment of varicocele, the most of which is of historical significance. At present, there is no consensus in favor of one or another method of surgical treatment of varicocele, which determines the relevance of further research.
Objective. To evaluate the effectiveness of a new minimally invasive method of surgical treatment of varicocele using the author's method.
Materials & methods. The study enrolled 763 patients aged 18 – 46 years (mean age 26.3 years) with varicocele who underwent testicular vein subinguinal ligation according to the author's technique. Inclusion criteria: varicocele grades 1 – 3, aged ≥ 18 years, semen abnormalities according to semen analysis and dilated spermatic cord veins according to ultrasound, retrograde blood flow according to Doppler ultrasound. Exclusion criteria: previously operated patients with recurrent varicocele, patients with May-Thurner syndrome and bilateral varicocele. The examination included eight control points: before surgery and 3, 6, 12, 24, 36, 48, and 60 months after surgery. Physical scrotal examination with Valsalva test, semen analysis, and Dopper scrotal ultrasound were performed at the control dates.
Results. The average surgery time was 15 min (10 – 30 min). All patients were discharged 1 to 2 days after surgery. At follow-up for 60 months, patients showed improvement in spermatogenesis / or no progression of semen abnormalities during follow-up after surgery based on clinical, laboratory and instrumental studies (semen analysis, ultrasound / Doppler ultrasound); no data on testicular hypotrophy, hydrocele were revealed. A scrotal haematoma was detected in one patient in the early postoperative period. Recurrent varicocele (1.4%) was detected in 11 patients during the follow-up period.
Conclusion. The technique is effective, easily reproducible, characterised by a low rate of recurrence and postoperative complications.
For citations:
Kyzlasov P.S., Abuev G.G., Mustafaev A.T., Bokov A.I. Novel patented minimally invasive technique for surgical treatment of varicocele: technique overview. Urology Herald. 2023;11(1):52-58. (In Russ.) https://doi.org/10.21886/2308-6424-2023-11-1-52-58
Introduction
Varicocele is a varicose (cluster-like) expansion of the veins of the plexus pampiniformis, which is accompanied by intermittent or permanent venous reflux [1]. The first mention of varicocele dates to the 1st century AD, when the ancient Roman scientist Aulus Cornelius Celsus described this disease and linked the expansion of the veins of the bund plexus and testicular atrophy on the same side. Since then and until now, varicocele remains an urgent problem [2][3]. Varicocele is the most common cause of male infertility [4–6]. The prevalence of this disease in the general population is approximately 15%; it is detected in 19–41% of men with primary infertility and 45–81% of men with secondary infertility [7].
According to Rotker et al., the frequency of varicocele recurrence varies widely and may depend on the studied population (for example, puberty or adult period), indications for surgical intervention (for example, testicular atrophy, infertility, or pain syndrome), the degree of initial varicocele (for example, subclinical or clinical), the surgical technique used (for example, open, laparoscopic or percutaneous access), criteria to determine relapse (for example, clinical or subclinical) and the follow-up period [8]. About 120 surgery types for varicocele are known worldwide, but most of them have only historical significance due to the high frequency of relapses [9–11].
The surgery proposed by the Argentine professor Oscar Ivanissevich became widely known at the beginning of the 20th century, as it was made in the form of subinguinal ligation of the testicular vein at the level of the intersection with the iliac vessels, since anatomically, the testicular vein in this area is most often represented by one branch. In 1960, after analysing the experience of varicocele surgical treatment using his own method, he defined varicocele as an anatomical and clinical syndrome anatomically characterised by varicose spermatic cord veins, and clinically by venous reflux [12].
However, given the high frequency of relapses, the search for an optimal intervention in varicocele continued. In the middle of the 20th century, Palomo (1949) presented the experience of surgical treatment of 40 patients with varicocele using his own technique, which consisted in retroperitoneal ligation of the testicular artery and vein 2 cm above the inner inguinal ring. He concluded that the testicle is supplied with blood by three arteries and ligation of one of them does not lead to hypotrophy [13]. In 1985, Marmar et al. presented the technique of microsurgical subinguinal ligation of all testicular vein branches, which to this day remains the “gold standard” in safety and efficacy [14].
Currently, the most used methods are laparoscopic ligation / coupling of the testicular vein (laparoscopic analogue of Ivanissevich technique), microsurgical subinguinal ligation of the testicular vein and endovascular phlebosclerosis of the testicular vein. The lack of a consensus in favor of one or another method of surgical treatment of varicocele leads to the search for new techniques, so the Urology and Andrology Centre, State Research Center Burnasyan Federal Medical Biophysical Center of Federal Medical Biological Agency introduced and clinically tested a method of surgical treatment, subsequently patented in 2021 [15].
The study aimed to evaluate the effectiveness of a new minimally invasive method of surgical treatment of varicocele, performed according to the author's method.
Materials and methods
The study included 763 patients who underwent subinguinal ligation of the testicular vein according to the author's method in the period from 2011 to 2021 in the Urology Division, Urology and Andrology Centre, State Research Center Burnasyan Federal Medical Biophysical Center of Federal Medical Biological Agency.
The inclusion criteria were as follows: patients with varicocele of degrees I–III aged 18–46 years, pathospermia according to the spermogram and enlarged veins of the pampiniformis plexus according to ultrasound, retrograde blood flow, according to dopplerometry of the vessels of the spermatic cord.
The exclusion criteria were as follows: previously operated patients with recurrent varicocele, patients with May-Thurner syndrome and bilateral varicocele.
Control points of examination: 0 – before surgery, 1 – 3 months after surgery, 2 – 6 months after surgery, 3 – 12 months after surgery, 4 – 24 months after surgery, 5 – 36 months after surgery, 6 – 48 months after surgery, 7 – 60 months after surgery. The standard medical examination included a physical examination of the scrotum organs with a Valsalva sample, a spermogram, and Dopper ultrasound of the scrotum organs.
The surgical intervention included the following stages:
- local infiltration skin anaesthesia, conduction anaesthesia of the spermatic cord (lidocaine solution, 1.0%) (Fig. 1);
- vertical incision of the scrotal skin 3–4 cm below the outer inguinal ring;
- layer-by-layer separation of the spermatic cord from the surrounding tissues;
- longitudinal dissection of the fascia of the spermatic cord (Fig. 2);
- displacement of the vas deferens with its accompanying artery and vein posteriorly (when the branches of the testicular artery are found, lateral displacement);
- ligation of the plexus pampiniformis veins with a single block with stitching, suture material 4/0 – 5/0 and their intersection, coagulation of small branches if necessary (Fig. 3);
- hemostasis control, layered suturing of the wound with nodular sutures;
- aseptic sticker, suspension on the scrotum.
In the postoperative period, during the day, cold is applied to the scrotum area in the mode of 30 minutes with a break of 1.5 hours.
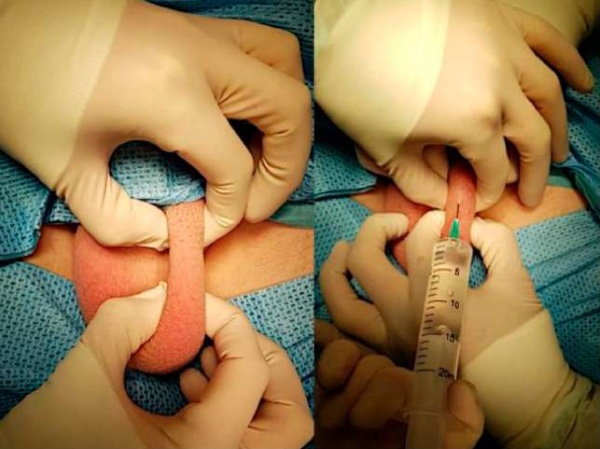
Figure 1. Local skin infiltration anesthesia and conductive anesthesia of the spermatic cord
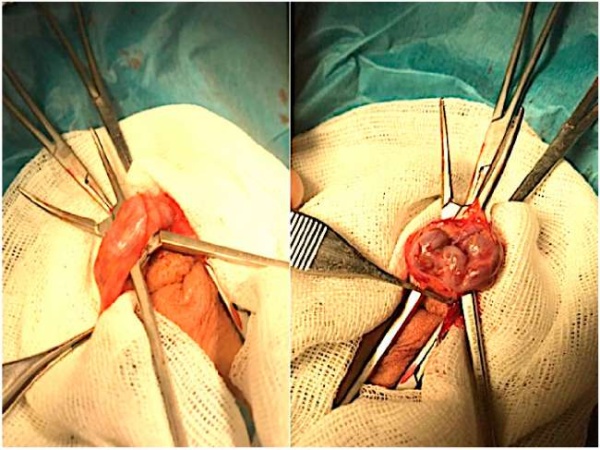
Figure 2. The spermatic cord was isolated in layers, its fascia was dissected longitudinally
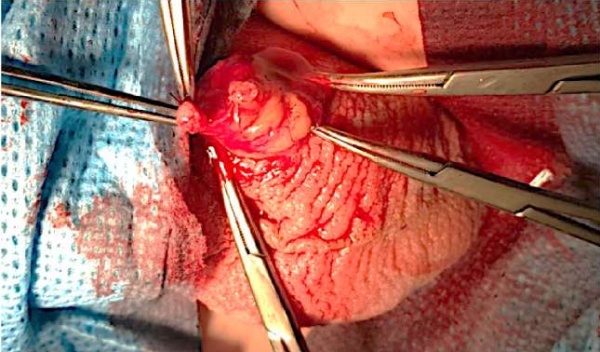
Figure 3. The pampiniform plexus veins are ligated en bloc and transected
Statistical analysis. Data processing was carried out using the Microsoft Excel 2019 software (Microsoft Corp., Redmond, WA, USA) and IBM SPSS Statistics 21.0 (SPSS: An IBM Company, IBM SPSS Corp., Armonk, NY, USA). The descriptive statistics of the age of patients and the surgery time were described in the form of a median (Me) with a description of the minimum and maximum indicators (min – max), discrete values — a percentage of occurrence (%).
Results
The median age of patients was 26.3 years (18–46 years). The distribution of patients according to the degree of varicocele (WHO classification): degree I – 20% (n = 152); degree II – 49% (n = 374); degree III – 31% (n = 237) (Fig. 4).
Before surgical treatment, pathospermia was observed in 96% of cases (n = 733) asthenoteratozoospermia (37.9%, n = 290), isolated teratozoospermia (34.6%, n = 265), oligoasthenoteratozoospermia (24.8%, n = 190), isolated oligospermia (2.3%, n = 18) were observed in most patients (Fig. 5).
The median surgery time was 15 minutes (10–30 minutes). All patients were discharged on the first to second day after surgery. In 1 patient in the early postoperative period, a scrotal haematoma was detected that did not require surgical treatment.
While monitoring patients for 5 years after surgical treatment according to clinical, laboratory and instrumental studies (spermogram, scrotal duplex ultrasound), no data on testicular hypotrophy or hydrocele were detected. Therefore, the improvement in spermatogenesis was noted in patients in the form of an increase in the average concentration of spermatozoa, total sperm motility, and a decrease in the number of pathological spermatozoa forms (Fig. 6). In 11 (1.4%) patients, a recurrence of varicocele was detected during the follow-up period.
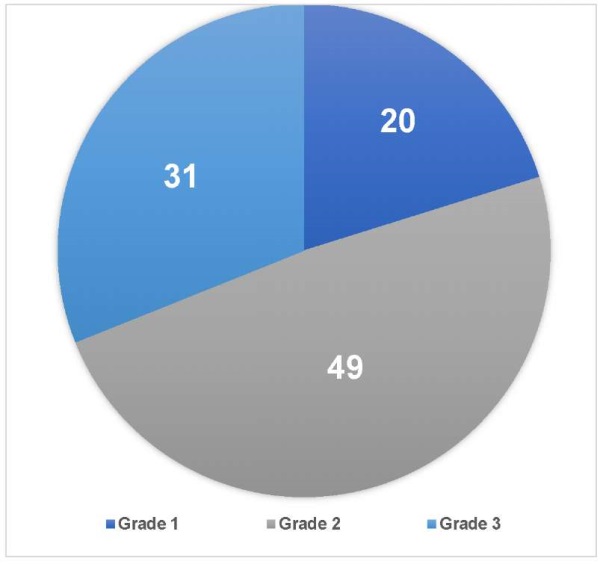
Figure 4. Varicocele grades in patients
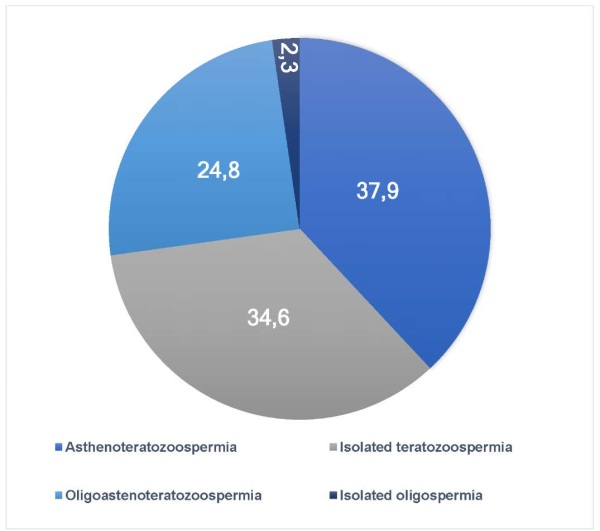
Figure 5. Semen abnormalities in patients before surgery
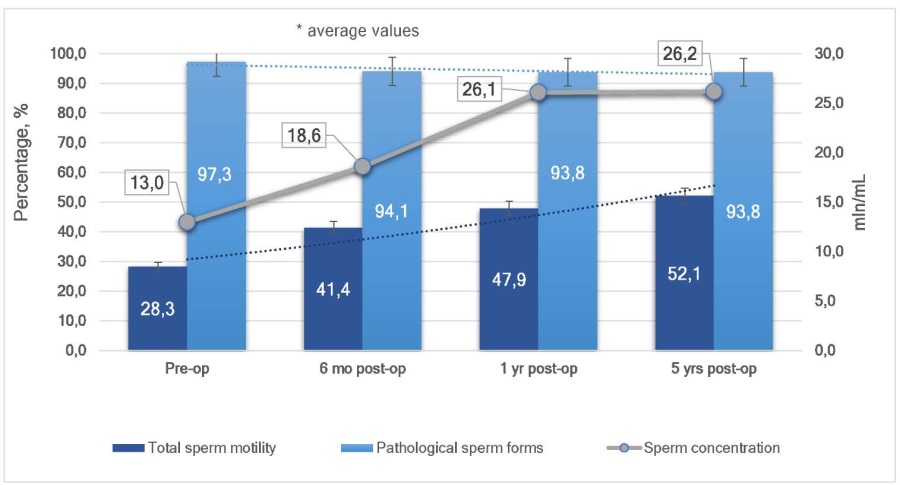
Figure 6. Dynamics of average semen parameters
Discussion
The knowledge of the spermatic cord elements anatomy, especially the testicular artery anatomy, is of great practical importance during the treatment process. The blood testicular supply is carried out by 3 groups of arteries that actively anastomose with each other: the testicular artery, the artery of the muscle that raises the testicle, and the artery of the vas deferens [16]. Jarish (1889) and Ebert (1904) in their works noted that the testicular artery in the scrotum is divided into 3 – 4 branches. Gilbo (1957) described that the testicular artery divides into 1 to 4 branches mainly at the posterior edge of the testicle at 3 cm above it, and no division was observed above 7 cm [17–19]. According to the results of a study by Pellanda (1903), four types of structure of the testicular artery are presented, depending on the division in the scrotal part of the spermatic cord: 1) division into two branches (75%); 2) division into 3 to 6 branches (15%); 3) the testicular artery goes with one trunk and does not give branches; 4) the testicular artery passes in the posterior part of the scrotal part of the spermatic cord into the mediastinum of the testicle, giving branches to the lateral surfaces of the testicle. He also believed that the testicular artery divides at 1 to 4 cm from the testicle [20]. According to Artyukhin (2004) and his study of 62 isolated anatomical complexes, including the testicle, its appendage, elements of the spermatic cord throughout, including the membranes, up to the inner inguinal ring, it is possible to conclude that the arterial system of the testicle was divided into three sections: inguinal, scrotal, directly testicle and its appendage. It was revealed that the testicular artery in the inguinal part of the spermatic cord is most often located in the thickness of the pampiniformis plexus, and branches rarely depart from the main artery. In the scrotal part of the spermatic cord, the testicular artery is often divided into small branches, single branches are in its anterior part [21].
Thus, during the subinguinal ligation of the testicular veins in the external inguinal ring, the possibility of injury to the testicular artery increases during the ligation of veins in this area.
Therefore, it is important to use an operating microscope and microsurgical instruments while performing subinguinal interventions, and to use them, undoubtedly, the skill of microsurgical interventions is necessary. The ligation of the plexus pampiniformis with a single block through the scrotal access is possible without the use of a microscope, which makes the operation reproducible, significantly reduces the operation time, and reduces the financial costs of surgical aid while ensuring a low percentage of relapse and postoperative complications.
Conclusion
The described technique is effective, easily reproducible, and characterised by a low frequency of relapses and postoperative complications.
References
1. Lopatkin N.A., ed. Urologija: nacional'noe rukovodstvo. Moscow: GJeOTAR-Media; 2011. (In Russian). ISBN: 978- 5-9704-1990-8.
2. Hotchkiss RS. Infertility in the male. In: Campbell MF, Harrison JH, eds. Urology. Philadelphia, USA: Saunders; 1970.
3. Petrochenkov E.V., Rostovskaya V.V. History of varicocele surgery. Russian Journal of Pediatric Surgery, Anesthesia and Intensive Care. 2018;8(4):88-96. (In Russian). DOI: 10.17816/psaic483
4. Nagler HM, Luntz RK, Martinis FG. Varicocele. In: Lipshultz LI, Howards SS, eds. Infertility in the male. St. Louis, MO: Mosby Year Book; 1997.
5. Kamischke A, Nieschlag E. Varicocele treatment in the light of evidence-based andrology. Hum Reprod Update. 2001;7(1):65-9. DOI: 10.1093/humupd/7.1.65
6. Agarwal A, Deepinder F, Cocuzza M, Agarwal R, Short RA, Sabanegh E, Marmar JL. Efficacy of varicocelectomy in improving semen parameters: new meta-analytical approach. Urology. 2007;70(3):532-8. DOI: 10.1016/j.urology.2007.04.011
7. Kibar Y, Seckin B, Erduran D. The effects of subinguinal varicocelectomy on Kruger morphology and semen parameters. J Urol. 2002;168(3):1071-4. DOI: 10.1097/01.ju.0000026956.70079.b6
8. Rotker K, Sigman M. Recurrent varicocele. Asian J Androl. 2016;18(2):229-33. DOI: 10.4103/1008-682X.171578
9. Beshliev D.A. Varikocele. Klassifikaciya, diagnostika, lechenie. Difficult Patient. 2007;5(12-13):9-13. (In Russian). eLIBRARY ID: 16861526; EDN: OEZMWH
10. Çoban S, Keleş I, Biyik I, Güzelsoy M, Türkoğlu AR, Özgünay T, Ocak N. Is there any relationship between mean platelet volume and varicocele? Andrologia. 2015;47(1):37-41. DOI: 10.1111/and.12220
11. Chen XF, Zhou LX, Liu YD, Ping P, Chen YH, Cao M, Sun J. [Comparative analysis of three different surgical approaches to varicocelectomy]. Zhonghua Nan Ke Xue. 2009;15(5):413-6. (In Chinese). PMID: 19514552
12. Ivanissevich O. Left varicocele due to reflux; experience with 4,470 operative cases in forty-two years. J Int Coll Surg. 1960;34:742-55. PMID: 13718224
13. Palomo A. Radical cure of varicocele by a new technique; preliminary report. J Urol. 1949;61(3):604-7. DOI: 10.1016/s0022-5347(17)69113-4
14. Patent № 2756019 C1 Rossijskaja Federacija, MPK A61B 17/00. Maloinvazivnyj metod hirurgicheskogo lechenija varicocele: № 2020133185: zajavl. 08.10.2020: opubl. 24.09.2021 / P.S. Kyzlasov, A.A. Kazhera, A.T. Mustafaev. (In Russian). URL: https://patenton.ru/patent/RU2756019C1
15. Marmar JL. The evolution and refinements of varicocele surgery. Asian J Androl. 2016;18(2):171-8. DOI: 10.4103/1008-682X.170866
16. Artjuhin A.A. Fundamental'nye osnovy sosudistoj andrologii: ucheb. posobie dlja stud. vyssh. ucheb. zavedenij. Moscow: Izdatel'skij centr «Akademija», 2008. (In Russian).
17. Jarisch A. Ueber die Schlagadern des menschlichen Hodens. Berichte des naturwissenschaftlichen-medizinischen Verein Innsbruck. 1889;18:32-79.
18. Ebert CJ. Die männlichen Geschlechtsorgane. Handbuch der Anatomie des Menschen. Jena, Fischer: 1904.
19. Gil'bo I.S. Arterii muzhskoj polovoj zhelezy cheloveka. Arh. Anatomii, gistologii i jembriologii. 1957;34(1):106-114. (In Russian).
20. Pellanda CH. La circulation artérielle du testicule. Int. Wschr. F. Anat. Physiol. 1903;20:240-266.
21. Artjuhin A.A. Anatomophysiological and clinical aspects of the testical arterial system. I.P. Pavlov russian medical biological herald. 2004;1-2:41-53. (In Russian). eLIBRARY ID: 9319056; EDN: HVYDWH
About the Authors
P. S. KyzlasovRussian Federation
Pavel S. Kyzlasov — M.D., Dr.Sc.(Med); Prof., Dept. of Urology and Andrology, Medical and Biological University of Innovation and Continuing Education;
Head, Urology and Andrology Centre,
Moscow
G. G. Abuev
Russian Federation
Gebek G. Abuev — M.D.; Postgrad. Student, Dept. of Urology and Andrology, Medical and Biological University of Innovation and Continuing Education;
Urologist, Urology Division, Urology and Andrology Centre,
Moscow
A. T. Mustafaev
Russian Federation
Ali T. Mustafayev — M.D.; Assist.Prof., Dept. of Urology and Andrology, Medical and Biological University of Innovation and Continuing Education;
Urologist, Urology Division, Urology and Andrology Centre,
Moscow
A. I. Bokov
Russian Federation
Aleksej I. Bokov — M.D., Cand.Sc.(Med); Urologist, Urology Division, Urology and Andrology Centre,
Moscow
Review
For citations:
Kyzlasov P.S., Abuev G.G., Mustafaev A.T., Bokov A.I. Novel patented minimally invasive technique for surgical treatment of varicocele: technique overview. Urology Herald. 2023;11(1):52-58. (In Russ.) https://doi.org/10.21886/2308-6424-2023-11-1-52-58













































