Scroll to:
Treatment of cryptorchidism in pediatric surgical practice: a multicenter study
https://doi.org/10.21886/2308-6424-2023-11-1-13-25
Abstract
Introduction. Cryptorchidism is a common disease in pediatric urological and andrological practice since the issues of tactical approaches and its optimal treatment remain extremely relevant. Cryptorchidism makes a significant contribution to the structure of male infertility.
Objective. To conduct a retrospective analysis of treatment results in children and adolescents with cryptorchidism.
Materials & methods. This study summarises the treatment results of 8308 patients with cryptorchidism aged from 6 months to 17 years who underwent inpatient treatment in the Russian Federation and the Republic of Uzbekistan.
Results. It was revealed that from 2015 to 2019, patients were admitted for surgical treatment evenly over the years. The ratio of right-sided / left-sided / bilateral cryptorchidism was 4.6 : 4.4 : 1 The inguinal form prevailed more than 6 times over the abdominal location. At the same time, 26.1% of the patients underwent surgery at the optimal time, and 9.8% were older than 10 years. More often, children are operated from an open inguinal access (95.0%), much less often — laparoscopically and percutaneously. Stage-by-stage treatment was carried out in 6.0% of patients.
Conclusion. Thus, the approach presented in the study in the surgical treatment of cryptorchidism provided good treatment results. The number of disease relapses was 1.9% (mainly among children over 7 years old). Most surgeons are very reserved about primary orchidectomies (only 3.8% were performed).
For citations:
Axelrov M.A., Minaev S.V., Razin M.P., Yusupov Sh.A., Tsap N.A., Tarakanov V.A., Shamsiev J.A., Karpova I.Yu., Smolentsev M.M., Sergienko T.V., Baturov M.A., Daniyarov E.S., Strizhenok D.S., Grigoruk E.H., Mikhalev O.Yu., Komarova S.Yu., Bykov N.I., Barova N.K., Trushin P.V., Gramzin A.V., Aslanov D.A., Grigorova A.N. Treatment of cryptorchidism in pediatric surgical practice: a multicenter study. Urology Herald. 2023;11(1):13-25. (In Russ.) https://doi.org/10.21886/2308-6424-2023-11-1-13-25
Introduction
Cryptorchidism is one of the systemic diseases accompanied by impaired testicular migration from the abdominal cavity to the scrotum [1–5]. Cryptorchidism can be diagnosed at any age; the incidence of the disease is 10.0–20.0% in newborns (up to 30.0% in premature newborns), up to 3.0% in 1-year-old children, 1.0% in puberty, and 0.3% in adult men [6–8].
The available academic literature data do not allow determining a single strategy for this defect treatment. This study was carried out to exchange the experience, as well as to unify and develop a common strategy for the treatment of cryptorchidism in children. Twelve paediatric surgical centres from ten regions of the CIS participated in this study (Tyumen, Yekaterinburg, Stavropol, Kirov, Kurgan, Krasnodar, Novosibirsk, Surgut, Nizhny Novgorod, and Samarkand (Republic of Uzbekistan)).
The study aimed to conduct a retrospective analysis of treatment results the cases of cryptorchidism in children and adolescents in large Russian pediatric surgical centers and the leading pediatric surgical clinic of Uzbekistan.
Materials and methods
Twelve paediatric surgical centres from ten CIS regions participated in this particular study: Tyumen Regional Clinical Hospital No. 2; Yekaterinburg Regional Children's Clinical Hospital and Yekaterinburg Children's City Clinical Hospital No. 9; Stavropol Regional Children's Clinical Hospital; Kirov Regional Children's Clinical Hospital; Red Cross Kurgan Regional Children's Clinical Hospital; Krasnodar Children's Regional Clinical Hospital; Novosibirsk Regional Clinical Hospital and Novosibirsk Children's City Clinical Hospital No. 1; Surgut District Clinical Hospital; Nizhny Novgorod Regional Children's Clinical Hospital; Samarkand Scientific Center of Pediatric Surgery, (Republic of Uzbekistan). Questionnaires sent to clinics included questions concerning the age of the operated children, forms of pathology, the side of the lesion, methods used to lower and fix the testicle, the results of surgical and conservative treatment of patients in this category, including long-term results, consequences, and cases of relapse.
Therefore, according to the questionnaires sent from these centers, a comparative analysis of the effectiveness of the treatment of cryptorchidism over the past 5 years (from 2015 to 2019) was carried out. Unfortunately, some of the questionnaires sent did not contain information on all the issues. Nevertheless, the analysis of the materials obtained, and their geography allowed to get a complete picture of the state and trends of surgical cryptorchidism treatment in two post-Soviet countries.
Statistical analysis. The statistical processing of the research results was carried out using the Statistica 10.0 (StatSoft Inc., Tulsa, OK, USA). The results were expressed in absolute and relative figures.
Results
During the past 5 years, 8308 children diagnosed with cryptorchidism have been operated on in the regions mentioned above (Tab. 1). Children with cryptorchidism in the illuminated perspective were admitted to clinics evenly. In total, a slight decrease was revealed in the number of children operated in 2019.
Table 1. Distribution of children by years of surgery
|
City |
Years |
Overall |
||||
|
2015 |
2016 |
2017 |
2018 |
2019 |
||
|
Yekaterinburg |
445 |
428 |
395 |
372 |
346 |
1986 |
|
Krasnodar |
320 |
278 |
418 |
318 |
326 |
1660 |
|
Kirov |
96 |
109 |
115 |
106 |
85 |
511 |
|
Kurgan |
73 |
59 |
79 |
55 |
48 |
314 |
|
N. Novgorod |
69 |
51 |
33 |
31 |
55 |
239 |
|
Novosibirsk |
195 |
215 |
203 |
211 |
199 |
1023 |
|
Stavropol |
– |
– |
164 |
208 |
186 |
558 |
|
Tyumen |
141 |
126 |
130 |
115 |
123 |
635 |
|
Samarkand |
276 |
236 |
241 |
315 |
126 |
1194 |
|
Surgut |
18 |
38 |
45 |
53 |
34 |
188 |
|
Overall |
1633 |
1540 |
1823 |
1784 |
1528 |
8308 |
Right-sided and left-sided localization of malformation occur with approximately the same frequency and make up a total of 45.8% and 43.8%, respectively. A two-way process was recorded in 10.5% of observations. However, in two regions (Stavropol and Samarkand), the frequency of two-sided cryptorchidism was noticeably higher than in other clinics, reaching 18.5% and 17.5%, respectively (Fig. 1).
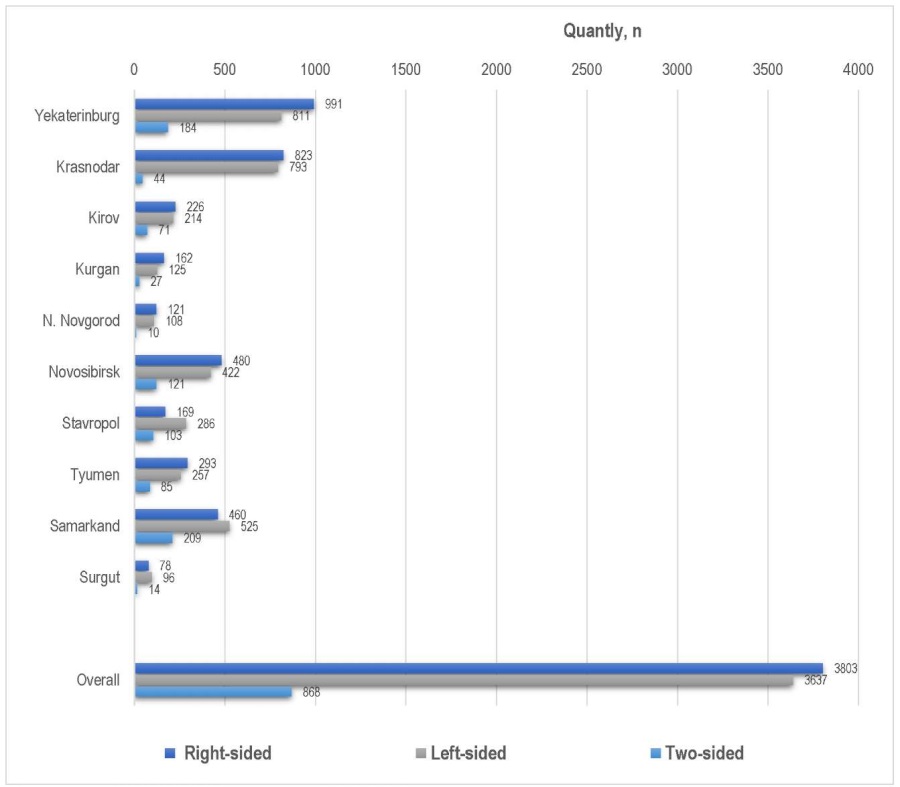
Figure 1. Sides of cryptorchidism localisation
According to the summary data, 86.3% of the children had an inguinal location of the testicle at the time of the initial operation and 13.7% of the children had a testicle located in the abdominal cavity. In all regions, most of the children had inguinal retention. It should be noted that in some regions, a large percentage of patients (38.4% in Stavropol and 24.7% in Tyumen) with an abdominal testicle location was recorded (Fig. 2).
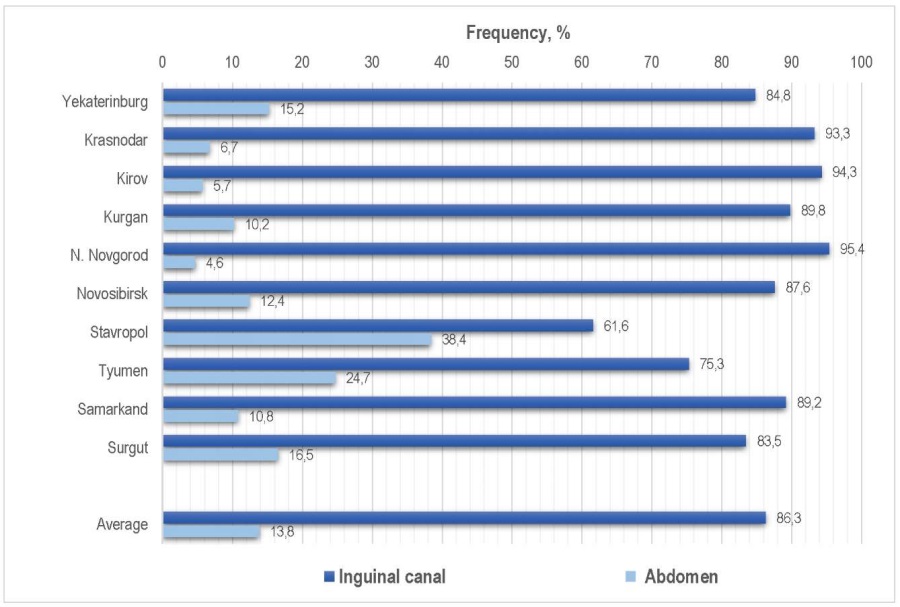
Figure 2. Testicular location in children with cryptorchidism
Table 2 shows the distribution of children by region and age of surgical intervention. At the same time, only 26.1% (2170) of children underwent surgery within the time frame recommended by the Russian Association of Pediatric Surgeons (and the WHO Committee of Experts). Most of the children (61.38 – 73.9%) go to the surgical table at the age of 2 years and 2951 (35.5%) boys were operated after 5 years of life.
Table 2. Distribution of children by age of surgery
|
City |
Age, years |
||||||||
|
<1 |
1–2 |
2–3 |
3–4 |
4–5 |
5–6 |
6–7 |
7–10 |
> 10 |
|
|
Yekaterinburg |
24 1.2% |
393 19.8% |
623 31.4% |
234 11.8% |
111 5.6% |
113 5.7% |
94 4.7% |
240 12.1% |
154 7.8% |
|
Krasnodar |
16 1.0% |
505 30.4% |
341 20.5% |
145 8.7% |
83 5.0% |
78 4.7% |
88 5.3% |
223 13.4% |
181 10.9% |
|
Kirov |
0 |
125 24.5% |
112 21.9% |
44 8.6% |
24 4.7% |
30 5.9% |
25 4.9% |
75 14.7% |
76 14.9% |
|
Kurgan |
14 4.5% |
80 25.5% |
50 15.9% |
31 9.9% |
21 6.7% |
4 1.3% |
14 4.5% |
23 67.6% |
77 24.5% |
|
N. Novgorod |
27 11.3% |
43 18.0% |
55 23% |
25 10.5% |
15 6.3% |
19 7.9% |
16 6.7% |
24 10.0% |
15 6.3% |
|
Novosibirsk |
25 2.4% |
367 35.9% |
165 16.1% |
103 10.1% |
69 6.7% |
57 5.6% |
63 6.2% |
101 9.9% |
73 7.1% |
|
Stavropol |
15 2.7% |
135 24.2% |
126 22.6% |
88 15.8% |
62 11.1% |
42 7.5% |
15 2.7% |
49 8.7% |
26 4.7% |
|
Tyumen |
50 7.9% |
248 39.1% |
83 13.1% |
33 5.2% |
30 4.7% |
27 4.3% |
30 4.7% |
67 10.2% |
67 10.2% |
|
Samarkand |
0 |
43 3.6% |
130 11.1% |
165 13.8% |
146 12.2% |
198 16.6% |
162 13.6% |
220 18.4% |
130 11.1% |
|
Surgut |
3 1.6% |
57 30.3% |
45 23.9% |
19 10.1% |
9 4.8% |
11 5.9% |
9 4.8% |
20 10.6% |
15 8.0% |
|
Overall |
174 2.1% |
1996 24.0% |
1730 20.8% |
887 10.7% |
570 6.9% |
579 7.0% |
516 6.2% |
1042 12.5% |
814 9.8% |
In most regions, during the studied years the conservative therapy was not used at all. Isolated medical examinations were available in Surgut (7 patients), Tyumen and Nizhny Novgorod (3 children each). According to the results of consultation and examination before the primary surgery, hormone therapy was prescribed by an endocrinologist for patients at the age of 1 to 2 years (4 children), at the age from 2 to 3 years (1 child), at the age from 3 to 4 years (1 boy), at the age from 7 to 10 years (5 children) and for patients older than 10 years (2 clinical cases). In Kirov, hormone therapy was prescribed only when the second stage of surgery was necessary, when it was initially impossible to lower the testicle to the scrotum. There were 10 children with such clinical cases, 6 children at the age of 1 to 2 years and 4 children at the age from 2 to 3 years. In addition, 5 of these children suffered a two-way process.
Petrivalsky-Schoemacker surgery is used by all the surveyed clinics as a choice surgery together with testicular fixation (less often) to the bottom of the scrotum (Schuller, Mixter). Transcrotal access by A. Bianchi was rarely used in the medical cases considered. In this very sample, only 3 paediatric surgical centres (Krasnodar, Tyumen, and Samarkand) used peritoneal access for testicular reduction and fixation. However, almost all centres used laparoscopy in the treatment of abdominal (227 children) and inguinal (102 children) cryptorchidism. Therefore, Table 3 shows the applied methods of orchiopexy by surgical centers.
Table 3. Distribution of children by types of surgery
|
City |
Open inguinal access |
Laparoscopy |
Scrotal access |
Overall |
||
|
canal |
abdomen |
canal |
abdomen |
|||
|
Yekaterinburg |
1678 |
171 |
7 |
130 |
– |
1986 |
|
Krasnodar |
1524 |
102 |
5 |
9 |
20 |
1660 |
|
Kirov |
482 |
17 |
– |
12 |
– |
511 |
|
Kurgan |
269 |
23 |
13 |
9 |
– |
314 |
|
N. Novgorod |
228 |
11 |
– |
– |
– |
239 |
|
Novosibirsk |
894 |
127 |
2 |
– |
– |
1023 |
|
Stavropol |
344 |
212 |
– |
2 |
– |
558 |
|
Tyumen |
340 |
101 |
71 |
56 |
67 |
635 |
|
Samarkand |
1061 |
129 |
– |
– |
4 |
1194 |
|
Surgut |
153 |
22 |
4 |
9 |
– |
188 |
|
Overall |
6973 83.9% |
915 11.0% |
102 1.2% |
227 2.8% |
91 1.1% |
8308 100% |
In this study, only in Samarkand, a two-stage approach to the surgical treatment of children with cryptorchidism was not used. It should be noted that not only the abdominal forms were treated in stages. With the inguinal location of the testicle, if the length of the deferens duct or vessels was insufficient and there was significant tension, surgeons in all the Russian clinics (493 observations) went to fix the testicle on the way to the scrotum, followed by the repeated surgery after 6 months. One hundred twenty-two children were operated on in Yekaterinburg, Krasnodar — 36, Kirov — 66, Kurgan — 6, Nizhny Novgorod — 8, Novosibirsk — 55, Tyumen — 19, Surgut — 23 patients. The largest number of two-stage surgeries was observed in Stavropol – 158. In these clinics, the testicle was lowered both for the first and second time from the inguinal access in 332 children. Moreover, in Nizhny Novgorod and Novosibirsk, this option of the two-stage relegation was the only one. In 130 patients, the first stage of surgical treatment consisted of laparoscopic mobilisation and the second was the final reduction and fixation of the inguinal access. In 31 patients, both stages were performed laparoscopically.
It is often revealed intraoperatively that the undescended testicle is not developed, and removal of the testicle rudiments may be required. The decision in all the clinics is made by a consultation gathered at the operating table with the involvement of the surgical service head of the hospital and the head of the department. Table 4 shows the distribution of children who required testicular removal by age.
Table 4. The number of cases of orchidectomy at primary surgery
|
City |
Age, years |
Overall |
||||||||
|
<1 |
1–2 |
2–3 |
3–4 |
4–5 |
5–6 |
6–7 |
7–10 |
>10 |
||
|
Yekaterinburg |
1 |
5 |
6 |
4 |
4 |
1 |
3 |
8 |
6 |
38 |
|
Krasnodar |
– |
59 |
39 |
14 |
9 |
14 |
18 |
5 |
8 |
166 |
|
Kirov |
– |
– |
– |
– |
– |
1 |
– |
– |
– |
1 |
|
Kurgan |
1 |
3 |
3 |
2 |
2 |
– |
– |
– |
– |
11 |
|
N. Novgorod |
– |
– |
– |
– |
– |
– |
– |
– |
– |
– |
|
Novosibirsk |
1 |
8 |
5 |
7 |
2 |
2 |
4 |
5 |
2 |
36 |
|
Stavropol |
– |
– |
– |
– |
– |
– |
– |
– |
– |
– |
|
Tyumen |
1 |
6 |
1 |
2 |
9 |
15 |
10 |
3 |
3 |
50 |
|
Samarkand |
– |
– |
– |
– |
– |
– |
– |
– |
– |
– |
|
Surgut |
– |
– |
1 |
4 |
– |
1 |
1 |
6 |
1 |
14 |
|
Overall |
4 |
81 |
55 |
33 |
26 |
34 |
36 |
27 |
20 |
316 |
As can be seen from the table, orchidectomy was performed during primary surgery in 316 (3.8%) children. The testicle was removed most often at the age of 1 to 2 years. This surgery was not carried out in Nizhny Novgorod, Stavropol, and Samarkand.
Table 5 shows the distribution of children suffering from recurrent cryptorchidism by age at the time of primary surgery. The authors of this study observed a recurrence of cryptorchidism in 160 (1.9%) children. There were no disease relapses during the analysed period in Stavropol only. Relapse is possible at any age, but it most often occurs in children operated at the age of 4 to 5 years (31 cases – 19.4%) and at the age older than 7 years (50 cases – 31.2%). In 91.9% of the cases, the recurrent testicle stopped in the inguinal canal, and only in 8.1% of the children the testicle returned to the abdominal cavity after medical intervention. Failures since the short vascular bundle of the testicle does not allow the testicle to be adequately lowered into the scrotum do not always end in relapse. As a result, the acute ischemic disorders may occur in the postoperative period, which often leads to gonad atrophy. From the summary data, it was found out that the removal of the testicle in the long-term period due to the development of hypoplasia and atrophy was required in 327 (3.9%) children. The most frequent removal of the testicle in the long-term postoperative period was performed in Samarkand (174 operations) and Novosibirsk (42).
Table 5. Number of repeated surgical interventions depending on age
|
City |
Age, years |
Overall |
||||||||
|
< 1 |
1–2 |
2–3 |
3–4 |
4–5 |
5–6 |
6–7 |
7–10 |
> 10 |
||
|
Yekaterinburg |
– |
7 |
6 |
1 |
2 |
– |
2 |
1 |
– |
19 |
|
Krasnodar |
– |
– |
– |
– |
1 |
– |
1 |
1 |
1 |
4 |
|
Kirov |
– |
1 |
1 |
1 |
2 |
– |
– |
1 |
10 |
9 |
|
Kurgan |
– |
1 |
– |
1 |
– |
– |
1 |
– |
2 |
5 |
|
N. Novgorod |
1 |
1 |
2 |
– |
– |
2 |
2 |
1 |
3 |
12 |
|
Novosibirsk |
– |
4 |
4 |
7 |
12 |
6 |
9 |
9 |
4 |
55 |
|
Stavropol |
– |
– |
– |
– |
– |
– |
– |
– |
– |
– |
|
Tyumen |
1 |
7 |
3 |
3 |
4 |
3 |
21 |
|||
|
Samarkand |
– |
1 |
3 |
2 |
7 |
2 |
3 |
2 |
1 |
21 |
|
Surgut |
– |
– |
1 |
4 |
– |
1 |
1 |
6 |
1 |
14 |
|
Overall |
2 1.3% |
15 9.4% |
17 10.6% |
16 10.0% |
31 19.4% |
14 8.8% |
22 13.8% |
25 15.6% |
25 15.6% |
160 1.9% |
Discussion
Progressive postnatal death of spermatogenic epithelium in undescended testicles leads to the fact that patients of this category often suffer from infertility [1]. That is why the optimal age for starting treatment of cryptorchidism is the period from 6 months to 2 years of a child's life [8]. In the large multicenter material analyzed in the present study, only slightly more than a quarter of patients were operated on at this decreed age, at a time when 35.0% were over the age of 5 years. This fact can be connected both with the problems of dispensary supervision and with the low social responsibility of parents who consciously do not take their children to planned surgery, as they do not know (and/or forget) that the proportion of male infertility ranges from 25.0% to 50.0% of all the causes of infertility. Approximately 6.0–8.0% of married men are infertile [9]. Maybe it is possible to agree with the opinion of sociologists about the underestimated level of “child love” characteristic of modern society in general [10]. However, the medical components of this complex problem remain indisputable: with cryptorchidism, oligoasthenoteratozoospermia is detected in 60.0% of the examined patients, asthenoteratozoospermia is detected in 25.0% of patients, and normozoospermia – in only 10.0% [11].
Treatment of cryptorchidism includes not only operative – also conservative measures are to be applied. Moreover, some authors recommend starting therapeutic measures with conservative methods, and if conservative therapy is ineffective, resorting to surgical treatment within 1 month [8][12][13]. In the present study, hormone therapy was not used often, and then rather as a prelude to the second act of staged surgical treatment.
All the clinics surveyed used Petrivalsky-Schoemacker as a choice surgery, which is consistent with the literature data. Its effectiveness reaches 90.0% (level of evidence A) [14]. Since in 80.0% of the cryptorchidism cases, the testicles are determined palpationally, Bianchi and Squire in 1989 proposed to carry out the reduction from high transcrotal access. The authors pay special attention to the treatment of the ungliterated vaginal peritoneum process, which may be absent in 24.0–43.0% of cryptorchidism [6]. Despite a significant number of publications in the foreign academic literature with positive (including long-term) results of surgery, this method is still rarely mentioned in major modern guidelines on paediatric surgery [15][16]. In this study, transcrotal surgical interventions had a small proportion, they were used only in three pediatric surgical centers (Krasnodar, Tyumen, and Samarkand). The situation with the use of laparoscopic techniques in the treatment of cryptorchidism in children appears somewhat different. In modern paediatric surgery and in the diagnosis and treatment of abdominal cryptorchidism, a breakthrough is simply associated with the introduction of laparoscopy. Currently, diagnostic laparoscopy can be called the “gold standard” for non-palpable testicles. Laparoscopy allows us not only to determine the location of the gonad, if it is visualised in the abdominal cavity, but also to choose an adequate surgical method of orchiopexy [7][17]. Laparoscopy was used by the authors of the study in the treatment of 227 children suffering from abdominal cryptorchidism and 102 boys with inguinal one.
Therefore, two-stage surgeries are performed in the cases with a high location of the testicle and insufficient length of vessels for simultaneous reduction. The stage approach has become more widespread in the cases of abdominal cryptorchidism form. Laparoscopic two-stage Fowler-Stephens surgery consists in the intersection (at the first stage) of the main vascular testicle bundle. After 6 months, the second stage of the surgery – relegation – is performed [18][19]. In the present study, two-stage surgeries were not performed only in Samarkand. After all, retraction of the stretched testicle is not uncommon, this complication is only observed in 29.1% of orchiopexies [20][21]. Furthermore, this condition is fraught with gonad atrophy, which can determine the need to remove an atrophied testicle. The most frequent removal of the testicle in the long-term postoperative period was carried out in Samarkand (174).
- According to the results of the study, the ratio of right-sided/left-sided/two-sided cryptorchidism was revealed as 4.6:4.4:1. The inguinal form of cryptorchidism prevailed over the abdominal one by more than 6 times.
- Only 26.1% of sick children are currently operated on within the prescribed optimal period, and 35.5% are older than 5 years.
- More often, children are operated from an open inguinal access (94.9%), much less often – laparoscopically (4.0%) and percutaneously (3.9%). About 6.0% of patients were subjected to step-by-step treatment. Hormone therapy as a method of treatment proved to be limited in use.
- The average number of diseases relapses according to the multicenter study was 1.9% (more often relapses occurred during surgical treatment of children over the age of 7 years).
- Most regions are extremely reserved about primary orchidectomy (it was performed only in 3.8% of patients). However, subsequent organ-resecting surgery was performed in another 3.9% of patients.
References
1. Hramova E.B., Aksel'rov M.A., SHajtarova A.V., Grigoruk E.H. Cryptorchidism in children: a Multidisciplinary problem. Tactics of specialists in the diagnosis and treatment of the disease. Medicinskaya nauka i obrazovanie Urala. 2018;19(3):174-179. (In Russian). eLIBRARY ID: 35686826; EDN: YATLHV
2. Batra NV, DeMarco RT, Bayne CE. A narrative review of the history and evidence-base for the timing of orchidopexy for cryptorchidism. J Pediatr Urol. 2021;17(2):239-245. DOI: 10.1016/j.jpurol.2021.01.013
3. Sizonov V.V., Makarov A.G., Kagantsov I.M., Kogan M.I. Cryptorchidism: a comprehensive assessment of the terminology and classification. Urology Herald. 2021;9(2):7-15. (In Russian). DOI: 10.21886/2308-6424-2021-9-2-7-15
4. Sharkov S.M., Vasileva I.G., Strelnikov A.I., Polozov V.V. Comparative characteristic of morphological changes and phenotypic markers of displasia of connective tissue in children with various urological and andrological pathology. Detskaya Khirurgya (Russian Journal of Pediatric Surgery). 2018;22(3):120-123. (In Russian). DOI: 10.18821/1560-9510-2018-22-3-120-123
5. Kalfa N, Veyrac C, Lopez M, Lopez C, Maurel A, Kaselas C, Sibai S, Arena F, Vaos G, Bréaud J, Merrot T, Kalfa D, Khochman I, Mironescu A, Minaev S, Avérous M, Galifer RB. Multicenter assessment of ultrasound of the spermatic cord in children with acute scrotum. J Urol. 2007;177(1):297- 301; discussion 301. DOI: 10.1016/j.juro.2006.08.128
6. Kogan M.I., Shaldenko O.A., Orlov V.M., Sizonov V.V. Historical aspects of modern methods for the surgical treatment of abdominal forms of cryptorchism. Russian Journal of Pediatric Surgery (Detskaya Khirurgiya). 2014;18(3):48-52. (In Russian). eLIBRARY ID: 21591635; EDN: QJGGPM
7. Faizulin A.K., Poddubnyi I.V., Fedorova E.V., Shkityr Z.V., Petrova M.G., Kolosova P.A. Treatment policy for children with different forms of cryptorchidism. Andrology and genital surgery. 2012;13(2):40-44. (In Russian). eLIBRARY ID: 17729657; EDN: OXZLAV
8. Kriptorhizm. Federal'nye klinicheskie rekomendacii. Moscow; 2015. (In Russian).
9. Spitz L., Coran A.G. Operative Pediatric Surgery. Taylor Francis Group, LLC; 2013.
10. Yanovsky K., Rusakova E., Tarapovskaya K., Zhavoronkov S., Cherny D., Sokol Y., Drobyshevskaya T., Kochetkova O., Mau V., Letunova T. Crisis of the Family Institution in the Post-Industrial Society: Analysis of Causes and and Ways for Overcoming. Nauchnye trudy. In-t ekonomiki perekhod. perioda. 2008;112. (In Russian). URL: https://cyberleninka.ru/article/n/krizis-instituta-semiv-postindustrialnom-obschestve-analiz-prichin-i-vozmozhnosti-preodoleniya
11. Steinbrecher H. The undescended testis: working towards a unified care pathway for 2014. Arch Dis Child. 2014;99(5):397-8. DOI: 10.1136/archdischild-2013-305459
12. Lee J, Kim Y, Jou S, Park C. 소아와 청소년의 서혜부와 음 낭 질환 [Inguinal and Scrotal Diseases in Children and Adolescents]. J Korean Soc Radiol. 2022;83(4):792-807. (In Korean). DOI: 10.3348/jksr.2021.0099
13. Ogaĭ S.V. Method of treatment of testicular hypoplasia by early. Medicinskij zhurnal Zapadnogo Kazahstana. 2012;1(33):48-49. (In Russian).
14. Menovshchikova L.B., Rudin YU.E., Garmanova T.N., SHaderkina V.A. Klinicheskie rekomendacii po detskoj urologiiandrologii. Moscow: Izdatel'stvo «Pero»; 2015. (In Russian).
15. Qin KR, Morley C, Nataraja RM, Pacilli M. The spectrum of testicular-epididymal fusion anomalies in children with cryptorchidism: Personal experience, systematic review and meta-analysis. J Pediatr Urol. 2020;16(2):124-129. DOI: 10.1016/j.jpurol.2019.12.016
16. Zvizdic Z, Aganovic A, Milisic E, Jonuzi A, Zvizdic D, Vranic S. Duration of symptoms is the only predictor of testicular salvage following testicular torsion in children: A casecontrol study. Am J Emerg Med. 2021;41:197-200. DOI: 10.1016/j.ajem.2020.11.023
17. Savchuk M.O., Pjattoev Ju.G. Through scrotal access when cryptorchidism in children. Russian journal of pediatric surgery, anesthesia and intensive care. 2012;2(3):51-53. (In Russian). eLIBRARY ID: 18634837; EDN: PRULGZ
18. Elder JS. Surgical Management of the Undescended Testis: Recent Advances and Controversies. Eur J Pediatr Surg. 2016;26(5):418-426. DOI: 10.1055/s-0036-1592197
19. Rusak PS, Voloshin YUL Minimally invasive methods of diagnosis and treatment of abdominal cryptorchidism. Medicinskaya nauka i obrazovanie Urala. 2016;17(3):22-26. (In Russian). eLIBRARY ID: 27039377, EDN: WTSGUJ
20. Minaev S.V., Bolotov Iu.N. Diagnosis and treatment children with acute scrotal pain. Twenty years single centre experiences. Medical News of North Caucasus. 2015;10(2):117- 120. (In Russian). DOI: 10.14300/mnnc.2015.10026
21. Panchenko I.A., Shipilov A.I. Surgical tactics of treatment of a cryptorchism in the specializes uroandrological center. Andrology and Genital Surgery. 2013;14(2):46-50. (In Russian). DOI: 10.17650/2070-9781-2013-2-46-50
About the Authors
M. A. AxelrovRussian Federation
Mikhail A. Axelrov — M.D., Dr.Sc.(Med), Full Prof.; Head, Dept. of Pediatric Surgery;
Head, Surgery Division No. 1,
Tyumen
S. V. Minaev
Russian Federation
Sergey V. Minaev — M.D., Dr.Sc.(Med), Full Prof.; Head, Dept. of Pediatric Surgery,
Stavropol
M. P. Razin
Russian Federation
Maxim P. Razin — M.D., Dr.Sc.(Med), Full Prof.; Head, Dept. of Pediatric Surgery,
Kirov
Sh. A. Yusupov
Russian Federation
Shuhrat A. Yusupov — M.D., Dr.Sc.(Med), Full Prof.; Head, Dept. of Pediatric Surgery # 1,
Samarkand
N. A. Tsap
Russian Federation
Natalya A. Tsap — M.D., Dr.Sc.(Med), Full Prof.; Head, Dept. of Pediatric Surgery,
Yekaterinburg
V. A. Tarakanov
Russian Federation
Viktor A. Tarakanov — M.D., Dr.Sc.(Med), Full Prof.; Prof., Dept. of Pediatric Surgery,
Krasnodar
J. A. Shamsiev
Russian Federation
Jamshid А. Shamsiev — M.D., Dr.Sc.(Med), Full Prof.; Head, Dept. of Pediatric Surgery # 2,
Samarkand
I. Yu. Karpova
Russian Federation
Irina Yu. Karpova — M.D., Dr.Sc.(Med); Prof., Dept. of Pediatric Surgery,
Nizhny Novgorod
M. M. Smolentsev
Russian Federation
Maxim M. Smolentsev — M.D., Сand.Sc.(Med); Senior Lecturer, Dept. of Hospital Surgery,
Surgut
T. V. Sergienko
Russian Federation
Tatyana V. Sergienko — M.D.; Postgrad. Student, Dept. of Pediatric Surgery,
Pediatric Surgeon, Surgery Division No.1,
Tyumen
M. A. Baturov
Russian Federation
Maxim A. Baturov — M.D.; Assist.Prof., Dept. of Pediatric Surgery,
Kirov
E. S. Daniyarov
Uzbekistan
Erkin S. Daniyarov — M.D.; Senior lecturer, Dept. of Pediatric Surgery # 2,
Samarkand
D. S. Strizhenok
Russian Federation
Dmitriy S. Strizhenok — M.D.; Head, Pediatric Surgery Division,
Nizhny Novgorod
E. H. Grigoruk
Russian Federation
Elvira H. Grigoruk — M.D.; Pediatric Urologist-Andrologist,
Tyumen
O. Yu. Mikhalev
Russian Federation
Oleg Yu. Mikhalev — M.D.; Assist.Prof., Dept. of Pediatric Surgery,
Krasnodar
S. Yu. Komarova
Russian Federation
Svetlana Yu. Komarova — M.D., Сand.Sc.(Med); Assoc. Prof., Dept. of Pediatric Surgery,
Pediatric Urologist-Andrologist, Pediatric Surgery Division No.2,
Yekaterinburg
N. I. Bykov
Russian Federation
Nikolai I. Bykov — M.D., Сand.Sc.(Med); Assist.Prof., Dept. of Pediatric Surgery,
Head, Surgery Division No.1,
Stavropol
N. K. Barova
Russian Federation
Natusya K. Barova — M.D., Сand.Sc.(Med); Head, Dept. of Pediatric Surgery,
Krasnodar
P. V. Trushin
Russian Federation
Pavel V. Trushin — M.D., Dr.Sc.(Med); Assoc.Prof., Dept. of Hospital and Pediatric Surgery,
Novosibirsk
A. V. Gramzin
Russian Federation
Aleksey V. Gramzin — M.D., Сand.Sc.(Med); Assoc.Prof., Dept. of Hospital and Pediatric Surgery,
Head, Pediatric Surgery Division,
Novosibirsk
D. A. Aslanov
Russian Federation
Dalgat A. Aslanov — M.D.; Head, Pediatric Surgery Division,
Kurgan
A. N. Grigorova
Russian Federation
Alina N. Grigorova — M.D.; Сand.Sc.(Med); Assist.Prof., Dept. of Pediatric Surgery,
Stavropol
Review
For citations:
Axelrov M.A., Minaev S.V., Razin M.P., Yusupov Sh.A., Tsap N.A., Tarakanov V.A., Shamsiev J.A., Karpova I.Yu., Smolentsev M.M., Sergienko T.V., Baturov M.A., Daniyarov E.S., Strizhenok D.S., Grigoruk E.H., Mikhalev O.Yu., Komarova S.Yu., Bykov N.I., Barova N.K., Trushin P.V., Gramzin A.V., Aslanov D.A., Grigorova A.N. Treatment of cryptorchidism in pediatric surgical practice: a multicenter study. Urology Herald. 2023;11(1):13-25. (In Russ.) https://doi.org/10.21886/2308-6424-2023-11-1-13-25













































