Scroll to:
Risk factors for re-infection in patients after drainage of the upper urinary tract due to obstructive pyelonephritis
https://doi.org/10.21886/2308-6424-2022-10-4-70-78
Abstract
Introduction. Reinfection after drainage of obstructive pyelonephritis exacerbates the postoperative course of the disease and delays the possible surgical intervention aimed at eliminating the cause of obstruction.
Objectives. To determine the percentage of re-infection in patients drained with double-J stent or nephrostomy catheter for obstructive pyelonephritis. To assess the relationship between the timing of drainage removal and development of re-infection. To establish risk factors for the development of re-infection.
Materials and methods. Medical records from 1022 patients who were treated from January 2019 to December 2021 and underwent drainage for obstructive pyelonephritis. The data in patients after nephrostomy and stenting were evaluated separately. A retrospective analysis of the time and frequency of the development of re-infection, as well as the effect of diabetes mellitus on pyelonephritis relapse, was carried out.
Results. Re-infection during drainage developed in 16 (4.8%) patients with a nephrostomy and 45 (6.5%) patients with a stent. Among those who had re-infection in the nephrostomy-group, 4 (25.0%) patients noted it within two weeks from the moment of drainage, and 11 (69.0%) at three-four weeks. In the stent-group, the number of patients who had a complication during the first two weeks was 15 (33.0%), and it was 22 (49.0%) during the next two weeks, The proportion of patients with diabetes mellitus was higher among those who developed pyelonephritis again.
Conclusion. The percentage of patients hospitalized with clinical re-infection after drainage of the upper urinary tract was 6.0%. There was an increase in the number of hospitalizations with recurrent pyelonephritis in cases where the drainage period lasted more than two weeks (p < 0.05).
For citations:
Mamaev I.E., Alekberov E.M., Glinin K.I., Saypulaev G.Sh., Kotov S.V. Risk factors for re-infection in patients after drainage of the upper urinary tract due to obstructive pyelonephritis. Urology Herald. 2022;10(4):70-78. (In Russ.) https://doi.org/10.21886/2308-6424-2022-10-4-70-78
Introduction
According to the guidelines of the European Association of Urologists and the American Urological Association, obstruction of the upper urinary tract (UUT) caused by a stone and resulting in the inflammatory process should be resolved by drainage with a ureteral stent or nephrostomy tube [1].
The installation of an internal ureteral stent is currently one of the most common drainage options for infectious and inflammatory diseases of the upper urinary tract (UUT), which are based on a violation of the urine passage [2]. Even though internal drainage with ureteral stents is an integral component of standard urological practice, their use is fraught with quite significant problems for the patient. Dysuria, lumbar and suprapubic pain, hematuria, and clinically manifest urinary tract infection (UTI) are present in most patients with an internal ureteral stent [3]. It is also known that ureteral stents in most cases are covered with bacterial biofilms sometime after installation, while sterile urine does not exclude bacterial colonization and the likely development of a subsequent clinical picture of UTI [4]. The internal drainage of the UUT, both for inflammatory diseases against the background of obstruction and after ureteropyeloscopy, by itself can lead to clinically significant recurrence of UTI, in particular pyelonephritis.
A similar situation occurs with inflammatory complications of persistent nephrostomy tubes. One of the important factors determining the likelihood of inflammatory complications against the background of urinary drainage is the duration of its stay [5]. There is evidence that up to 14% of patients demonstrate clinically significant UTI within 30 days of their initial diagnosis [6]. However, the authors do not provide data on the risk of pyelonephritis at different time periods within a month, which would be appropriate.
The study aimed to conduct a retrospective assessment of the relationship between the timing of drainage of the upper urinary tract with a stent or nephrostomy tube, as well as the presence of a concomitant disease such as diabetes mellitus in the patient with the development of acute pyelonephritis before drainage removal.
Materials and methods
In the course of this study, a retrospective evaluation was carried out: the authors used the data of patients who underwent UUT drainage with an internal stent or nephrostomy drainage for obstructive pyelonephritis, who were on in-patient treatment at Buyanov Moscow City Clinical Hospital — Moscow Healthcare Department in the period from January 1, 2019 to December 31, 2021. Demographic and clinical data of the patients were collected according to the analysis of electronic medical records. The following indicators were evaluated: gender, age, cause of obstruction, drainage method, presence and nature of urinary microbiota, presence of diabetes mellitus (DM), and timing of drainage removal. Separately, the number of patients who had a relapse of the clinical form of upper urinary tract infection that developed before drainage removal was recorded in cases where this led to unscheduled hospitalization. In this group, in addition to the above, the timing of the development of inflammatory complications was calculated against the background of drainage.
Inclusion criteria: the study included patients with a confirmed diagnosis of acute obstructive pyelonephritis who underwent UUT drainage. On discharge, all patients were informed in writing about the need to seek urological help within a month after drainage to remove drainage.
Exclusion criteria: bilateral process with the need for bilateral drainage, sepsis, urinary tract obstruction against the background of persistent malignant neoplasm, lack of documentary evidence of the fact of stent removal, patient death.
To diagnose acute obstructive pyelonephritis, a combination of the following indicators was used: local pain, fever, leukocytosis, an increase of C-reactive protein, dilation of the renal collecting system during an ultrasound examination.
A two-loop polyurethane ureteral stent 7 Ch (“Coloplast A/S”, Humlebæk, Denmark) with a length of 26 or 28 cm, depending on the patient's height, was used as internal drainage; a Kolibri puncture kit with a Vortek J-type catheter with a diameter of 10 Ch (“Coloplast A/S”, Humlebæk, Denmark) was used for nephrostomy.
In a microbiological study, the concentration of microorganisms ≥104 CFU/ml was considered a clinically significant titer.
The conditions for discharge from hospital were a combination of the following factors: absence of fever, adequate drainage function, absence of significant hematuria, tendency to decrease leukocytosis and CRP, as well as subjective improvement in the patient’s well-being.
The standard recommendation when transferring patients to outpatient treatment was to continue antibacterial therapy for a period of 5–7 days and perform native computed tomography of the UUT, followed by seeking advice for 2 weeks.
The issue of the subsequent disposal of urinary drainage was solved based on computed tomography or antegrade pyeloureterography. In the presence of a concretion, its removal was performed. In the case when the stone was not detected and there were no reasons to assume other causes of obstruction, the drainage was removed. In patients with nephrostomy, removal was preceded by antegrade pyeloureterography. The evaluation of the timing of the completion of drainage in both groups was carried out.
A separate category includes patients who had a clinical recurrence of urinary tract infection against the background of drainage. The same indicators used above for the diagnosis of obstructive pyelonephritis were used as criteria for clinical relapse, apart from dilation of the renal collecting system. In this cohort, both the time of onset of the complication and the characteristics of the patients available in medical records were studied, the evaluation of which may be prognostic significant from the point of view of the occurrence of the described complication (gender, age, the presence of DM and the nature of the pathogen).
Statistical analysis. Statistical processing of the data obtained was carried out using the PAST ver. 4.09 software package (Hammer et al., 2001). The data were tested for normality of the distribution using the Shapiro-Wilk and Kolmogorov-Smirnov methods. The calculation of the Kramer association coefficient and the Mann-Whitney U criterion were used. The differences were considered statistically significant at p < 0.05.
Results
During the period from January 2019 to December 2021, 1114 patients with unilateral obstructive pyelonephritis, unrelated to oncological obstruction, were drained with a ureteral stent or nephrostomy tube in the urological department of Buyanov Moscow City Clinical Hospital. Eighty-seven of them could not be examined, and 5 of them died for reasons unrelated to urological pathology. Thus, 1022 (432 men and 590 women) patients were directly included in the study, who underwent UUT drainage with a nephrostomy or an internal ureteral stent to decompress UUT in obstructive pyelonephritis. The patients were divided into 2 groups: group 1 — 690 patients who were drained with a ureteral stent and group 2 — 332 patients who underwent nephrostomy as a drainage method. The characteristics of patients are presented in Table 1.
Table 1. Primary patient demographics
|
Characteristics |
Group 1 |
Group 2 |
|
Age, years M ± SD |
55.2 ± 15.6 |
56.1 ± 14.9 |
|
Male, n |
242 |
213 |
|
Female, n |
448 |
119 |
|
Average bed-day after drainage |
3.3 |
3.5 |
|
Diabetes mellitus, n (%) |
163 (23.6%) |
52 (15.7%) |
The average age of patients in the groups practically did not differ — it was 55.2 and 56.1 years. As for the sex distribution, it differed very significantly: in the group of patients with a stent, there was an almost two-fold predominance of women (448 versus 242 men), and among those who had a nephrostomy tube, the inverse proportion was observed (211 men versus 119 women).
More than half of the patients in both groups had no bacterial growth in the urine obtained during the kidney drainage intervention. While assessing the clinically significant titer, it was revealed that the pathogens listed below were most often sown. In group 1, Enterococcus faecalis was detected in 83 patients (12.0%), Escherichia coli — in 79 (11.4%) patients, and Klebsiella pneumoniae — in 21 (3.0%) patients. In group 2, the distribution was as follows: E. faecalis was identified in 37 (11.1%) patients, E. coli — in 40 (12.0%), and K. pneumoniae — in 11 (3.3%) patients. Furthermore, in both groups of patients, the growth of Pseudomonas aeruginosa, Staphylococcus epidermidis, and Candida albicans was determined, but the proportion of these pathogens in the total mass did not exceed 1.0% (Table 2).
Table 2. Primarily identified microorganisms
|
Identified microorganisms, ≥104 CFU/ml |
Group 1 |
Group 2 |
|
n (%) |
||
|
Enterococcus faecalis |
83 (12.0%) |
37 (11.1%) |
|
Escherichia coli |
79 (11.4%) |
40 (12.0%) |
|
Klebsiella pneumoniae |
21 (3.0%) |
11 (3.3%) |
It took an average of 3.3 days in group 1 and 3.5 days in group 2 to achieve the criteria corresponding to the possibility of transferring the patient to an outpatient mode of continuing therapy after drainage was installed.
The timing of drainage removal is shown in Figure 1.
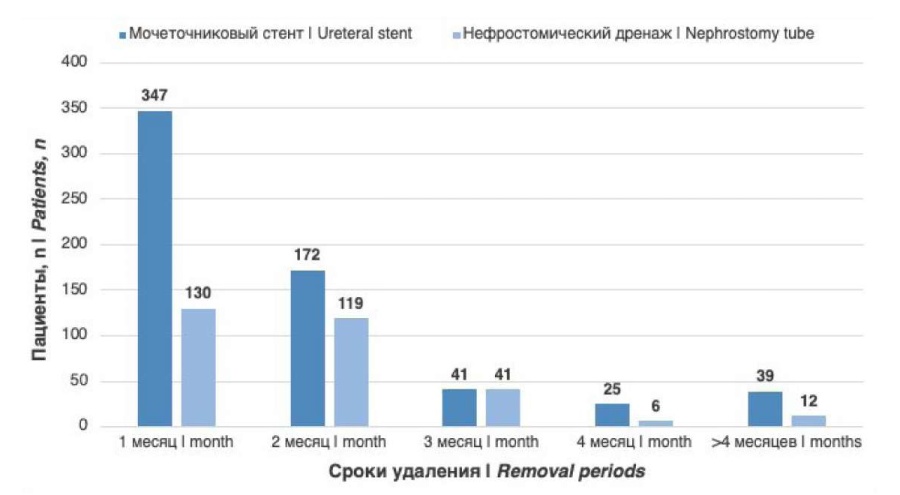
Figure 1. Timing of ureteral stent and nephrostomy tube removal
One of the most significant indicators was the number of patients who had a clinical recurrence of UTI in the form of acute pyelonephritis during their stay with drainage. Sixty-one (6.0%) patients were re-hospitalized with a picture of clinically significant re-infection. At the same time, there were 45 (6.5%) patients in the stent group and 16 (4.8%) patients in the nephrostomy group. The timing of the development of the complication by group is shown in Figure 2.
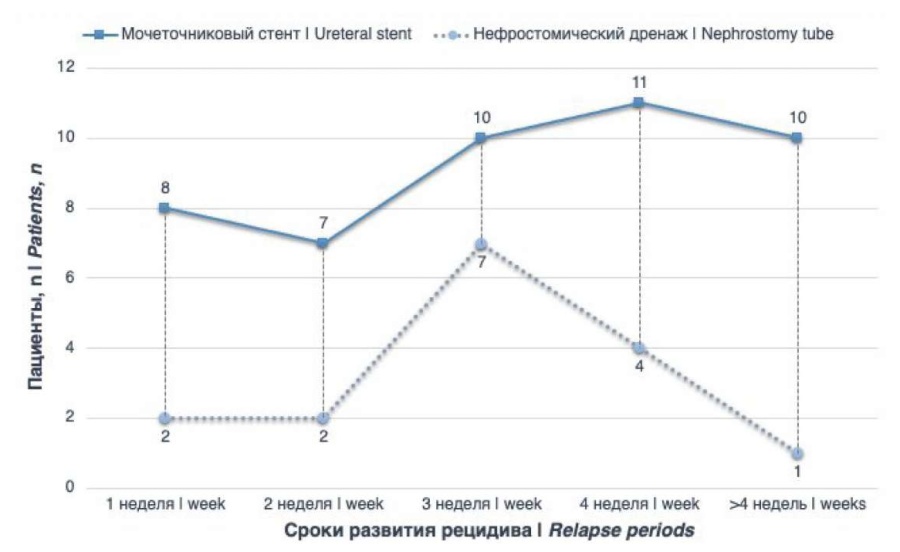
Figure 2. Timing of pyelonephritis relapse in patients with ureteral stent and nephrostomy drainage
Also, changes were noted in bacterial growth in patients with the symptoms of re-infection. The fact of microbial growth in a clinically significant titer was observed in 38 (62.0%) patients (Table 3).
Table 3. Identified microorganisms in re-infection
|
Identified microorganisms, ≥104 CFU/ml |
Group 1 |
Group 2 |
|
n (%) |
||
|
Enterococcus faecalis |
9 (19.6%) |
5 (31.3%) |
|
Escherichia coli |
4 (8.7%) |
1 (6.3%) |
|
Pseudomonas aeruginosa |
4 (8.7%) |
2 (12.5%) |
|
Klebsiella pneumonia |
3 (6.5%) |
2 (12.5%) |
|
Acinetobacter baumanii |
1 (2.2%) |
2 (12.5%) |
|
Staphylococcus epidermidis |
1 (2.2%) |
2 (12.5%) |
|
Candida albicans |
2 (4.3%) |
– |
In the group of patients with a ureteral stent, 163 (23.6%) patients suffered from DM, while among patients who underwent nephrostomy, there were 52 (15.7%). However, among those who demonstrated re-infection, the proportion of those who had a diagnosis of DM was already different: these were 15 (33.3%) patients in the group of patients with a ureteral stent and 3 (18.8%) patients in the group with a nephrostomy tube.
It is also obvious that the ratio of the microorganisms most frequently detected changed: if in group 1, the initial detection rates of E. faecalis and E. coli were comparable (12.0% and 11.4%), then in patients with re-infection, the ratio changed in favor of E. faecalis (19.6% and 8.7%). In group 2, the situation was similar, only with an even greater difference: the initial identification frequency was 11.1% in E. faecalis, 12% in E. coli, and 31.3% and 6.3% in re-infection, respectively. In addition, the proportion of typically hospital-acquired pathogens of P. aeruginosa increased significantly in patients hospitalized with the symptoms of re-infection.
Discussion
The first thing that attracts attention when assessing the composition of groups is the difference in the sex ratio of patients draining with a stent and a nephrostomy tube. The medical specialist often suggests installing a stent for women and nephrostomy drainage for men. There are two factors at the heart — the possibility to dispense with the use of local anesthesia during rigid cystoscopy in women and the risk of vesicoureteral reflux in the presence of infravesical obstruction in men.
During primary drainage in both groups, the proportion of positive urine culture studies obtained during drainage was no more than 35.0%. Yoshimura et al. (2005) demonstrate a similar result in their study [7]. At the same time, the data from most studies indicate the predominance of E. coli, which correlates with the results in the nephrostomy group; however, in the stenting group, E. faecalis prevailed slightly in the patients included in this study.
In the case of re-infection, the situation changes. In stent-patients, E. faecalis prevailed more than twice (19.6%) over other pathogens, and bacteriology study, in those with nephrostomy drainage, still demonstrated the predominance of E. coli (34.0%).
Nowadays, there is no evidence regarding the standards for the duration of drainage before subsequent lithotripsy [8]. According to Shi et al. (2016), based on an assessment of the dynamics of leukocytosis, leukocyturia and the presence of positive urine culture, in most cases, seven days of stent drainage after obstructive pyelonephritis are sufficient to safely perform an intervention to remove the concretion [9]. Itami et al. (2021), based on a retrospective assessment of the rate of stent colonization and the frequency of postoperative complications, concluded that an interval of 7–21 days could be considered optimal [10]. However, in practice, the time interval between drainage and lithotripsy can be longer. As can be seen in Figs. 1 and 2, at least half of the patients remove the stent no earlier than a month after its installation. With nephrostomy drains, the situation is even less favorable: the number of patients who eliminate drainage in the second month is almost equal to that in the first, and there are also many who have a nephrostomy for 3–4 months. According to authors’ opinion, this difference between the groups is based on two factors. The first is significant discomfort caused by an internal stent. Stent-associated symptoms stimulate the patient to remove drainage as soon as possible. The second factor is the comparatively better compliance of female patients, and the latter, as can be seen, significantly prevail in group 1.
The proportion of cases of clinically significant re-infection in this study was 6.5% in group 1 and 4.8% in group 2. In general, this is a relatively low indicator. For example, in the study by Kord et al. (2011), 28.0% of patients were hospitalized with re-infection after stent placement [11]. However, in this study, it is worth remembering the imperfection of the retrospective study and understanding that drained patients with pyelonephritis could be hospitalized in other medical institutions and not considered. Nevertheless, the difference in the proportion of patients who had re-infection in the stent group and in the nephrostomy group is minimal.
An important aspect of the assessment of patients with re-infection is the period of its development from the moment of drainage. As can be seen in Figs. 3 and 4, in group 1, the increase in the number of complications begins in the third week and, having reached a maximum in the fourth, goes into a state of a descending plateau. In group 2, the maximum re-infection occurs in the third week, followed by a decrease. There are various reasons to explain such dynamics. As a rule, taking antibiotics ends in the second week after the drainage is installed. The development of bacteriuria and the formation of biofilms on the surface of drains are important. According to Shabeena et al. (2018), more than 20.0% of patients have both after the day 15 from the moment of stent installation [3]. Pathogens such as E. coli and E. faecalis are known to begin to form a biofilm on drainage within the first 24 hours [12][13]. Biofilm formation on drainage means that antibiotic prophylaxis will not be able to provide sanitation of the urinary tract until drainage is removed; nevertheless, Kehinde et al. (2002) recommend antibiotic prophylaxis during stent removal, explaining this for reasons of preventing bacteremia [14].
The increase in the level of clinically significant re-infection, beginning at the third week of drainage, is probably the most significant indicator demonstrated in this study. For both groups, a comparison of the risk of complications at 1 – 2 weeks and at 3 – 4 weeks demonstrated a statistically significant relationship between the time elapsed after implantation and the risk of re-infection (p < 0.05).
Similar data were demonstrated in a study by Coskun et al. (2011), devoted to the assessment of early removal of a ureteral stent in patients who underwent kidney transplantation; the authors believe that stent removal two weeks after surgery reduces the frequency of infectious and inflammatory complications [15].
As in the case of other infectious and inflammatory diseases, the presence of DM in a patient is considered a risk factor for re-infection. If in group 1, there were 23.6% of patients with DM, then among those who had re-infection, the proportion of those was already 33.3%. Among patients from group 2, 15.7% suffered from DM, and the proportion of those who had DM among those who were re-hospitalized with pyelonephritis was 18.8%. The relationship between hyperglycemia and re-infection in patients with a ureteral stent was demonstrated in the work by Kord et al. (2019) [16]. Nevertheless, in this study, the difference in the absolute numbers of re-infection in patients with and without DM was not statistically significant in any of the groups (p = 0.344).
There were also no signs of a relationship between the parameters of gender, age of patients, and the nature of the pathogen during initial treatment with the frequency of re-infection in this study.
Conclusion
The main conclusion that the data obtained allow drawing is the need to reduce the time to drainage of the urinary tract for obstructive pyelonephritis to two weeks for most patients.
It is obvious that additional studies will be advisable to confirm the safety of lithotripsy at an earlier date after pyelonephritis, as well as to identify groups of patients who require an individual approach both in terms of drainage timing and position of preparation for surgery.
References
1. Assimos D, Krambeck A, Miller NL, Monga M, Murad MH, Nelson CP, Pace KT, Pais VM Jr, Pearle MS, Preminger GM, Razvi H, Shah O, Matlaga BR. Surgical Management of Stones: American Urological Association/Endourological Society Guideline, PART I. J Urol. 2016;196(4):1153-60. https://doi.org/10.1016/j.juro.2016.05.090
2. Kehinde EO, Al-Awadi KA, Tawheed A, Al-Hunayan A, Ali Y, Mahmoud AH. Factors affecting the fate of prolonged forgotten 'J' stents. Scand J Urol Nephrol. 2001;35(3):222-7. https://doi.org/10.1080/003655901750292006
3. Shabeena KS, Bhargava R, Manzoor MAP, Mujeeburahiman M. Characteristics of bacterial colonization after indwelling double-J ureteral stents for different time duration. Urol Ann. 2018;10(1):71-75. https://doi.org/10.4103/UA.UA_158_17
4. Zumstein V, Betschart P, Buhmann MT, Albrich WC, Nolte O, Güsewell S, Engeler DS, Schmid HP, Ren Q, Abt D. Detection of microbial colonization of the urinary tract of patients prior to secondary ureterorenoscopy is highly variable between different types of assessment: results of a prospective observational study. Biofouling. 2019;35(10):1083-1092. https://doi.org/10.1080/08927014.2019.1692000
5. Hanna B, Zhuo K, Chalasani V, Vass J, Rasiah K, Wines M, Vaux K, Chung A. Association between ureteric stent dwell time and urinary tract infection. ANZ J Surg. 2021;91(1-2):187-191. https://doi.org/10.1111/ans.16414
6. Szvalb AD, El Haddad H, Rolston KV, Sabir SH, Jiang Y, Raad II, Viola GM. Risk factors for recurrent percutaneous nephrostomy catheter-related infections. Infection. 2019;47(2):239-245. https://doi.org/10.1007/s15010-018-1245-y
7. Yoshimura K, Utsunomiya N, Ichioka K, Ueda N, Matsui Y, Terai A. Emergency drainage for urosepsis associated with upper urinary tract calculi. J Urol. 2005;173(2):458-62. https://doi.org/10.1097/01.ju.0000150512.40102.bb
8. Swonke ML, Mahmoud AM, Farran EJ, Dafashy TJ, Kerr PS, Kosarek CD, Sonstein J. Early Stone Manipulation in Urinary Tract Infection Associated with Obstructing Nephrolithiasis. Case Rep Urol. 2018;2018:2303492. https://doi.org/10.1155/2018/2303492
9. Shi YF, Li WG, Zhang J, Xia SJ, Sun XW. [Effect of double-J stent indwelling time in treatment of ureteric calculi complicated with infection]. Zhonghua Yi Xue Za Zhi. 2016;96(32):2588-91. (In Chinese) https://doi.org/10.3760/cma.j.issn.0376-2491.2016.32.015
10. Itami Y, Miyake M, Owari T, Iwamoto T, Gotoh D, Momose H, Fujimoto K, Hirao S. Optimal timing of ureteroscopic lithotripsy after the initial drainage treatment and risk factors for postoperative febrile urinary tract infection in patients with obstructive pyelonephritis: a retrospective study. BMC Urol. 2021;21(1):10. https://doi.org/10.1186/s12894-020-00754-8
11. Kord E, Siegel Y, Cooper A, Hirsh S, Goltsman G, Zisman A. Risk factors for re‐infection in patients drained with DJ stent for ureterolithiasis and sepsis. J Urol. 2017;197(4S):e1006. https://doi.org/10.1016/j.juro.2017.02.2157
12. Stickler DJ. Bacterial biofilms in patients with indwelling urinary catheters. Nat Clin Pract Urol. 2008;5(11):598-608. https://doi.org/10.1038/ncpuro1231
13. Gabi M, Hefermehl L, Lukic D, Zahn R, Vörös J, Eberli D. Electrical microcurrent to prevent conditioning film and bacterial adhesion to urological stents. Urol Res. 2011;39(2):81-8. https://doi.org/10.1007/s00240-010-0284-3
14. Kehinde EO, Rotimi VO, Al-Awadi KA, Abdul-Halim H, Boland F, Al-Hunayan A, Pazhoor A. Factors predisposing to urinary tract infection after J ureteral stent insertion. J Urol. 2002;167(3):1334-7. PMID: 11832726
15. Coskun AK, Harlak A, Ozer T, Eyitilen T, Yigit T, Demirbaş S, Uzar Aİ, Kozak O, Cetiner S. Is removal of the stent at the end of 2 weeks helpful to reduce infectious or urologic complications after renal transplantation? Transplant Proc. 2011;43(3):813-5. https://doi.org/10.1016/j.transproceed.2010.11.016
16. Kord E, Siegel YI, Goltsman G, Hirsh S, Zisman A. Risk factors for recurrent infection in patients drained with a DJ stent for ureterolithiasis and sepsis. J Urol. 2019;201(4S):е172. https://doi.org/10.1097/01.JU.0000555203.51979.44
About the Authors
I. E. MamaevРоссия
Ibragim E. Mamaev — M.D., Cand.Sc.(Med), Assoc. Prof. (Docent), Dept. of Urology and An-drology, Pirogov Russian National Research Medical University (Pirogov Medical University); Head, Urology Division, Buyanov Moscow City Clinical Hospital — Moscow Healthcare Department.
1 Ostrovityanova St., Moscow, 117997; 26 Bakinskaya St., Moscow, 115560
Competing Interests:
The authors declare no conflicts of interest
E. M. Alekberov
Россия
Emil M. Alekberov — M.D., Resident, Dept. of Urology and Andrology, Pirogov Russian National Research Medical University (Pirogov Medical University); Urologist, Urology Division, Buyanov Moscow City Clinical Hospital — Moscow Healthcare Department.
1 Ostrovityanova St., Moscow, 117997; 26 Bakinskaya St., Moscow, 115560
Competing Interests:
The authors declare no conflicts of interest
K. I. Glinin
Россия
Kirill I. Glinin — M.D., Assist.Prof., Dept. of Urology and Andrology, Pirogov Russian National Research Medical University (Pirogov Medical University); Urologist, Urology Division, Buyanov Moscow City Clinical Hospital — Moscow Healthcare Department.
1 Ostrovityanova St., Moscow, 117997; 26 Bakinskaya St., Moscow, 115560
Competing Interests:
The authors declare no conflicts of interest
G. Sh. Saypulaev
Россия
Gadzhimurad Sh. Saipulaev — M.D., Urologist, Urology Division, Buyanov Moscow City Clinical Hospital — Moscow Healthcare Department.
26 Bakinskaya St., Moscow, 115560
Competing Interests:
The authors declare no conflicts of interest
S. V. Kotov
Россия
Sergey V. Kotov — M.D., Dr.Sc.(Med), Full Prof., Head, Dept. of Urology and Andrology, Pirogov Russian National Research Medical University (Pirogov Medical University).
1 Ostrovityanova St., Moscow, 117997
Competing Interests:
The authors declare no conflicts of interest
Review
For citations:
Mamaev I.E., Alekberov E.M., Glinin K.I., Saypulaev G.Sh., Kotov S.V. Risk factors for re-infection in patients after drainage of the upper urinary tract due to obstructive pyelonephritis. Urology Herald. 2022;10(4):70-78. (In Russ.) https://doi.org/10.21886/2308-6424-2022-10-4-70-78
JATS XML













































