Scroll to:
Lower urinary tract symptoms following discontinuation of long-term non-medical use of testosterone preparations
https://doi.org/10.21886/2308-6424-2022-10-3-05-12
Abstract
Introduction. The aging process in men is accompanied by a progressive decrease in the level of serum testosterone (Tc). In addition to chronological aging, various factors contribute to the decline in testosterone levels. One of such factors contributing to the decrease in endogenous Tc and the development of secondary hypogonadism is the long-term use of testosterone preparations (TPs) used for non-medical purposes.
Objective. To assess the nature of lower urinary tract symptoms following discontinuation of long-term non-medical use of testosterone preparations.
Materials and methods. A clinical and statistical analysis of examination results in 31 men aged 22 – 46 years who received TPs for non-medical purposes while visiting gyms and subsequently turned to urologist with complaints of lower urinary tract symptoms (LUTS) was carried out. The study used the International Prostatic Symptom Score (IPSS) questionnaire, laboratory and instrumental examinations: general urine examination, general blood examination, prostate secretion microscopy, evaluation of serum total Tc, follicle-stimulating and luteinizing hormones, prolactin, estradiol, prostate ultrasound and bladder ultrasound, uroflowmetry
Results. When assessing LUTS, the prevalence of irritative symptoms was noted. The level of serum total Tc in 13 (41.9%) men was in the range of 8 – 11 nmol/l, in 18 (58.1%) men it was below 8 nmol/l. In addition, most patients (77.4%) had areas of reduced blood flow in the prostate, and 67.7% had prostate fibrosis.
Conclusion. Discontinuation of the use of long-term non-medical TPs can lead to the development of secondary hypogonadism and LUTS, which in most cases are irritative. In the treatment of these patients, an interdisciplinary rehabilitation program should be developed.
For citations:
Ibishev Kh.S., Sharbabchiev V.A., Paleny A.I., Uzhakhov M.M., Mezhidova A.D. Lower urinary tract symptoms following discontinuation of long-term non-medical use of testosterone preparations. Urology Herald. 2022;10(3):5-12. (In Russ.) https://doi.org/10.21886/2308-6424-2022-10-3-05-12
INTRODUCTION
The aging process in men is accompanied by a progressive decrease in serum testosterone (Ts) level [1][2]. In addition to chronological aging, various somatic diseases (diabetes mellitus, arterial hypertension, obesity, etc.) and some pharmacological drugs used to treat these conditions (atenolol, anapriline, verospiron, hypothiazid, etc.) contribute to a decline in circulating Ts levels [2–6]. In eugonadal men, transitory hypogonadotropic hypogonadism can develop because of any severe acute disease or injury [7][8]. In addition, harmful habits (smoking, drug addiction, alcohol abuse) and eating behavior (from malnutrition to obesity) increase age-related decrease in androgen levels. For these reasons, diseases associated with Ts deficiency are frequently diagnosed in young men.
A widely discussed issue among the factors that decrease endogenous Ts levels in young people is the long-term non-medical use of testosterone preparations (TPs) [9][10]. Risk groups for non-medical application of Ts include amateur sportsmen and people who train in sports centers for recreational physical activity [11][12].
Long-term TP application models, including supratherapeutic doses and TPs combinations, with further discontinuation, increase the risk of unfavorable psychological and other Ts-deficiency-associated complications. Consumers of TPs for non-medical purposes more often apply to physicians for non-psychiatric medical complications than for changes in their psychological status. At the same time, despite the unfavorable consequences, the motivation for the constant application of TPs is mainly maintained by psychological factors [12].
The most common adverse events for the urinary tract and reproductive organs associated with discontinuation of long-term intake of TPs, which inhibit endogenous Ts synthesis, include erectile dysfunction, decreased libido, infertility, and lower urinary tract symptoms (LUTS) [11][13][14].
The study aimed to evaluate the lower urinary tract symptoms character in men after the discontinuation of long-term non-medical use of testosterone preparations.
MATERIALS AND METHODS
The clinical-statistical analysis included the examination results of 31 men aged 22–46 years old, who received TPs for non-medical use during training in the gym and referred to a urologist with complaints about LUTS. TP intake was initiated without medical indications by men or sports centers personnel. Men developed LUTS after the discontinuation of TPs intake. Medical records said that before TPs usage, the hormonal status (Ts, follicle-stimulating hormone (FSH), luteinizing hormone (LH), prolactin, estradiol) agreed with the reference values. There were no signs of the infectious-inflammatory process of the urinary tract and prostate. Ten men took TPs for 2 years (32.3%), eight men – for 2 – 4 years (25.8%), and 13 men – for over 4 years (41.9%).
The examination of patients included the International Prostatic Symptom Score Scale (IPSS). For each patient, the total LUTS score was calculated (max score = 35). Additionally, storage symptoms (max score 20) and voiding symptoms (max score 15) were evaluated separately. Participants underwent laboratory and instrumental examinations: general urine examination, general blood examination, prostate secretion microscopy, evaluation of serum total Ts, FSH, LH, prolactin, estradiol, prostate and bladder ultrasound, uroflowmetry.
Hormonal tests were performed with a fully automated Cobas 6000 immunochemical analyzer («Roche Diagnostics International Ltd.», Rotkreuz, Switzerland), an innovative patented electrochemiluminescence (ECL) technology and a quantitative antigen assessment method based on changes in the signal of ECL before and after immunoreaction.
Statistical analysis. The study results were processed using Microsoft Excel tables from the software package Microsoft Office, 2007. Statistical analysis of the data was performed using the Statistica ver.6.1 software («StatSoft Inc.», Tulsa, OK, USA). The normality of the distribution was evaluated using the Shapiro-Wilk test. All qualitative data were described as the mean (M) ± standard deviation (SD). Qualitative data were described with absolute values (n) and percent (%).
RESULTS
Clinical and laboratory parameters gathered when the participants first referred for medical help are presented in the Table.
Table. Clinical and laboratory indicators
|
Indicators |
Value |
Reference |
|
|
Mean (M) |
Standard deviation (SD) |
||
|
Age, years |
37.96 |
4.43 |
– |
|
Тs, nmol/l |
13.82 |
4.19 |
≥ 12.10 |
|
FSH, mIU/ml |
7.41 |
4.07 |
0.70 – 11.20 |
|
LH, U/l |
8.21 |
3.22 |
1.14 – 8.75 |
|
Prolactin, µIU/ml |
205.00 |
36.21 |
86.00 – 324.00 |
|
Estradiol, pmol/l |
63.19 |
9.21 |
40.00 – 161.00 |
|
PSA, ng/ml |
1.21 |
0.44 |
≤ 4.00 |
|
Leukocytes in urine, x/ |
2.85 |
1.01 |
0.00 – 3.00 |
|
Leukocytes in EPS, x/ |
4.06 |
1.05 |
≤ 10.00 |
|
Prostate volume, cm3 |
34.19 |
5.07 |
≤ 25.00 – 30.00 |
|
Qmax, ml/s |
14.18 |
2.40 |
> 15.00 |
|
Residual urine, ml |
24.15 |
10.11 |
< 50.00 |
|
IPSS scale |
0 – 7 mild 8 – 19 moderate ≥ 20 severe |
||
|
Irritative symptoms, score |
8.87 |
3.06 |
|
|
Obstructive symptoms, score |
2.61 |
1.35 |
|
|
Total score |
11.51 |
4.13 |
|
|
Note. Ts — total testosterone; FSH — follicle-stimulating hormone; LH — luteinizing hormone; PSA — prostate-specific antigen; EPS — expressed prostatic secretion; IPSS — International Prostatic Symptom Score scale |
|||
IPSS score analysis showed that 27 (87.1%) patients had moderate symptoms (8–9 score) and 4 (12.9%) patients had light symptoms (0–7 score) (Fig. 1). The evaluation of the LUTS character showed that patients had primarily irritative symptoms by the number of cases and expression (Figs. 2, 3)
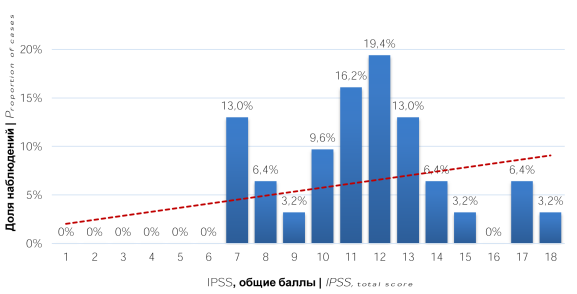
Figure 1. Distribution of patients by IPSS scores (total scores)
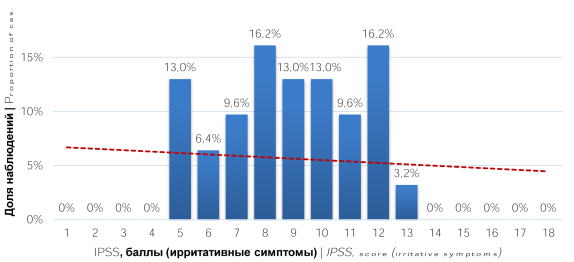
Figure 2. Distribution of patients by IPSS scores (irritative symptoms)
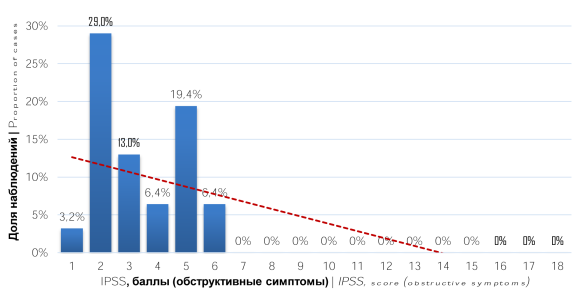
Figure 3. Distribution of patients by IPSS scores (obstructive symptoms)
In 13 (41.9%) patients, total Ts in serum was 8–11 nmol/L, in 18 (58.1%) patients, it was < 8 nmol/L. An increase in FHS levels was higher than the reference values in 5 (16.1%) men, LH and prolactin – in 9 (29.0%) and 5 (16.1%) men, respectively. A decrease in the estradiol level below the reference values was revealed in 6 (19.4%) men.
Prostate US revealed low blood flow areas in 24 (77.4%) cases: 11 (35.5%) unilateral localizations and 13 bilateral localizations (Fig. 4A). In 8 (25.8%) patients, these areas visualized in the transitory zone, and 4 (12.9%) patients — in the central zone, and 12 (38.7%) patients — in both prostate zones. Additionally, 21 (67.7%) patients had prostate fibrosis. In 7 (22.6%) patients, fibrosis was revealed in the single prostate lobe, and in 14 (45.2%) patients — in both lobes (Fig. 4B, 4C).
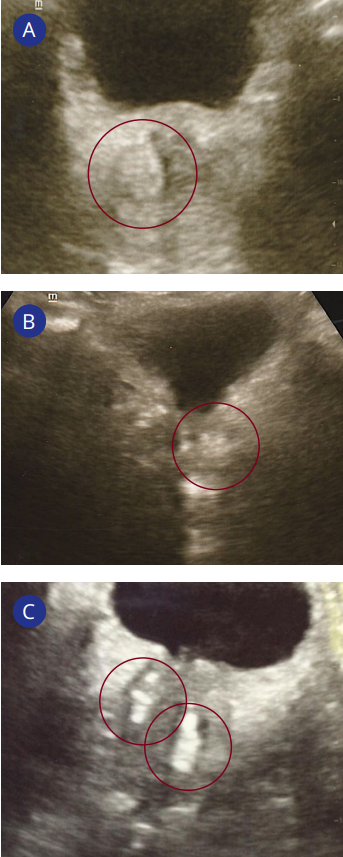
Figure 4. Prostate ultrasound scans: A — low blood flow area in the prostate right lobe; B — fibrosis in the prostate left lobe; C — fibrosis in prostate both lobes
DISCUSSION
There are few publications on pathogenetic mechanisms of adverse events in patients who received long-term therapy with TPs, including for the urinary tract and reproductive organs. However, it is known that the pathogenesis of LUTS associated with Ts deficiency has complicated neuroendocrine mechanisms, and endothelial dysfunction is the leading one. Ts deficiency is associated with a decrease or complete loss of endothelial cells capacity to provide an adequate synthesis of vasoconstricting and vasodilating factors that determine the structural-functional integrity of the endothelium and preventive anti-atherogenic effects [15][16]. Furthermore, it was shown that the functional activity of the detrusor, prostate, and urethra decreased in men with a Ts deficiency. In the conditions of a long-term decrease in serum Ts levels, the synthesis of nitrogen oxide (NO) is impaired in the vascular neuroendothelium, which leads to a persistent spasm of vascular walls in various organs and systems. This contributes to the development of vascular and cellular-tissue hypoxia. Additionally, local, and systemic ischemia (in particular, pelvic ischemia) develops, leading to hypoxia of the pelvic, urethral, and prostatic areas, which is considered the most important inducer of LUTS [13].
LUTS is an important determinant of the quality of life of any aged men [17][18]. In the present study, men, who used TPs for non-medical purposes for a long time, were primarily at the young age (aged 18 – 44 years) group (87.1%). In all cases, the registered LUTS had an irritative character. In 24 (77.4%) cases, they were combined with voiding symptoms. The total score of irritative symptoms in 22 (71.0%) patients was > 7 points, and in 9 (29.0%) patients, 5–7 points. The total score of obstructive symptoms in the examined men was < 7. In 77.4% of the patients, low blood flow and avascular areas were detected in the prostate, which are US signs of ischemia and could be the initiators of the clinical manifestation of LUTS. Additionally, in 29.0% of men, a Ts decrease and other hormone levels was registered, which are important links in the functioning of the urinary and reproductive organs.
CONCLUSION
Men who receive TPs for non-medical purposes for a long time develop secondary hypogonadism associated with adverse events for urinary tracts and reproductive organs. LUTS are one such adverse event that worsens the quality of life of men after discontinuation of TPs intake. They have a primarily irritative character and are caused by hypovascular and avascular changes in the prostate transitory and central zones, which should be considered before the indication of the required therapy. Furthermore, an interdisciplinary system of therapeutic measures should be proposed for such patients.
References
1. Wu FC, Tajar A, Pye SR, Silman AJ, Finn JD, O'Neill TW, Bartfai G, Casanueva F, Forti G, Giwercman A, Huhtaniemi IT, Kula K, Punab M, Boonen S, Vanderschueren D; European Male Aging Study Group. Hypothalamic-pituitary-testicular axis disruptions in older men are differentially linked to age and modifiable risk factors: the European Male Aging Study. J Clin Endocrinol Metab. 2008;93(7):2737-45. https://doi.org/10.1210/jc.2007-1972
2. Kogan MI, Vorobiev SV, Khripun IA, Belousov II, Ibishev KhS. Testosterone: from sexuality to metabolic control. Rostov-on-Don: Phoenix; 2017 (In Russ.)
3. Gusova Z.R., Dzantieva E.O. Importance of Visceral Obesity and Testosterone Deficiency in the formation of metabolic disorders in men. Urology Herald. 2019;7(3):14-22. (In Russ.) https://doi.org/10.21886/2308-6424-2019-7-3-14-22
4. Kuzmenko A.V., Kuzmenko V.V., Gyaurgiev T.A., Protsenko A.A., Shishonkova N.S. Erectile dysfunction because of psychological and somatic diseases in men of different age groups. Trends Dev Sci Edu. 2020;61(1) 44-47. (In Russ.) https://doi.org/10.18411/lj-05-2020-11
5. Mekhtiev TV, Mamedov MN. Treatment of age androgen deficiency with patients suffering from diabetes type 2. Resort medicine. 2015;2;122-6. (In Russ.) eLIBRARY ID: 24284561 EDN: ULKXBT
6. Khripun IA, Vorobyev SV, Morgunov MN, Belousov II, Dzantieva EO, Gusova ZR, Ibishev KhS, Kogan MI. The genetic aspects of endothelial dysfunction in patients with type 2 diabetes mellitus. Medical News of North Caucasus. 2015;10(4):339-43. (In Russ.) https://doi.org/10.14300/mnnc.2015.10083
7. Kogan MI, Ibishev KhS. Secondary hypogonadism in patients with damage to the urethra. Consilium Medicum. 2007;9(4):50-54. (In Russ.) URL: https://consilium.orscience.ru/2075-1753/article/view/92348
8. Ibishev K.S., Prokop J.O. New coronavirus disease 2019 (COVID-19): Is there an impact on male reproductive health. Urology Herald. 2022;10(1):128-134. (In Russ.)
9. https://doi.org/10.21886/2308-6424-2022-10-1-128-134
10. Isidori AM, Lenzi A. Risk factors for androgen decline in older males: lifestyle, chronic diseases and drugs. J. Endocrinol Invest. 2005;28(3):14-22. PMID: 16042355
11. Robertson C, Link CL, Onel E, Mazzetta C, Keech M, Hobbs R, Fourcade R, Kiemeney L, Lee C, Boyle P, McKinlay JB. The impact of lower urinary tract symptoms and comorbidities on quality of life: the BACH and UREPIK studies. BJU Int. 2007 Feb;99(2):347-54. https://doi.org/10.1111/j.1464-410X.2007.06609.x
12. Ibishev KhS, Volkova NI, Gusova ZR, Evseev PA, Sharbabchiev VA, Kogan MI. Genitourinary adverse events in men using non-medical testosterone preparations. Urologiia. 2022;(3):92-97. (In Russ.) https://doi.org/10.18565/urology.2022.3.92-97
13. Brower KJ. Anabolic steroid abuse and dependence in clinical practice. Phys Sportsmed. 2009;37(4):131-40. https://doi.org/10.3810/psm.2009.12.1751
14. Tyuzikov IA. Pathogenetic mechanisms of testosterone deficiency influence on lower urinary tract symptoms in men. Effective pharmacotherapy. 2020;16(20):32-42. (In Russ.) https://doi.org/10.33978/2307-3586-2020-16-20-32-42
15. Lykhonosov M.P., Babenko A.Y., Makarin V.A., Fedotov Yu.N. Peculiarity of recovery of the hypothalamic-pituitary-gonadal (hpg) axis, in men after using androgenic anabolic steroids. Problems of Endocrinology. 2020;66(1):104-12. (In Russ.) https://doi.org/10.14341/probl12223
16. Hotta Y, Kataoka T, Kimura K. Testosterone Deficiency and Endothelial Dysfunction: Nitric Oxide, Asymmetric Dimethylarginine, and Endothelial Progenitor Cells. Sex Med Rev. 2019;7(4):661-8. https://doi.org/10.1016/j.sxmr.2019.02.005
17. Traish AM, Johansen V. Impact of Testosterone Deficiency and Testosterone Therapy on Lower Urinary Tract Symptoms in Men with Metabolic Syndrome. World J Mens Health. 2018;36(3):199-222. https://doi.org/10.5534/wjmh.180032
18. Dudarev V.A., Startsev V.Yu., Baksheeva E.G. Clinical implications of using questionnaires in elderly men with urinary disorders. Urology Herald. 2020;8(4):23-31. (In Russ.) https://doi.org/10.21886/2308-6424-2020-8-4-23-31
19. Yassin AA, El-Sakka AI, Saad F, Gooren LJ. Lower urinary-tract symptoms and testosterone in elderly men. World J Urol. 2008;26(4):359-64. https://doi.org/10.1007/s00345-008-0284-x
About the Authors
Kh. S. IbishevRussian Federation
Khalid S. Ibishev — M.D., Dr.Sc.(Med), Assoc. Prof. (Docent); Prof., Dept. of Urology and Human Reproductive Health (with the Pediatric Urology and Andrology Course)
29 Nakhichevanskiy Ln., Rostov-on-Don, 344022, Russian Federation
V. A. Sharbabchiev
Russian Federation
Vladislav А. Sharbabchiev — M.D., Urologist
1 Lenin St., Mikhailovsk, 356240, Russian Federation
A. I. Paleny
Russian Federation
Andrey I. Paleny — M.D., Assistant, Dept. of Ultrasound Diagnostics
29 Nakhichevanskiy Ln., Rostov-on-Don, 344022, Russian Federation
M.-Kh. M. Uzhakhov
Russian Federation
Magomed-Khadzhi M. Uzhakhov — M.D, Urologist; Postgraduate student; Dept. of Urology and Human Reproductive Health (with the Pediatric Urology and Andrology Course)
29 Nakhichevanskiy Ln., Rostov-on-Don, 344022, Russian Federation
A. D. Mezhidova
Russian Federation
Anita D. Mezhidova — M.D., Ultrasound Practitioner
34 Peshkova St., Rostov-on-Don, 344023, Russian Federation
Review
For citations:
Ibishev Kh.S., Sharbabchiev V.A., Paleny A.I., Uzhakhov M.M., Mezhidova A.D. Lower urinary tract symptoms following discontinuation of long-term non-medical use of testosterone preparations. Urology Herald. 2022;10(3):5-12. (In Russ.) https://doi.org/10.21886/2308-6424-2022-10-3-05-12













































