Scroll to:
Alternative trans-parenchymal access for percutaneous contact nephrolithotripsy
https://doi.org/10.21886/2308-6424-2022-10-1-32-41
Abstract
Introduction. An actual issue of modern endoscopic surgery for urolithiasis is the development of techniques for optimal access to the stone. Percutaneous access during contact nephrolithotripsy (PCNL) is believed to reach the pyelocalyceal system (PCS) along the shortest trajectory and pass through the small calyces. It assumes multi-accessibility, as well as interventional cascading. Anatomically, the kidney is divided into five relatively independent segments in terms of blood supply. The thickness of the posterior one is only a quarter of the thickness of the kidney, which allows us to assume a significantly smaller number of vessels in this segment even outside the Zondek (Brödel) bloodless line.
Purpose of the study.To prove the possibility of using an optimized transparenchymal approach in PCNL based on the renal vascular structure.
Material and methods. A prospective analysis of the treatment of 41 patients with urolithiasis who hadPCNL. Before surgery, patients were randomized by gender, age, average stone size, and urolithiasis forms. Subjects were divided into two groups. Group 1 (study) —20 (48.8%) patients underwent PCNL through trans-parenchymal access to the inferior-lateral parts of the pelvis or the large lower renal calyx due to the ventral orientation of the lower small calyces. Group 2 (control) — 21 (51.2%) patients underwent standard PCNL. The creation of access to PCS was provided simultaneously with Doppler ultrasound of the renal vessels to prevent damage to the segmental and interlobular vessels of the kidney.
Results. In 73.2% of patients, the blood supply in the region of standard access to the PCS goes through the posterior segmental artery, which does not supply blood to the lower half of the kidney (type 1 blood supply). In 26.8% of patients, branches of the posterior segmental artery cross the projection of the inferior calyces (type 2 blood supply). In cases where it is impossible to perform a standard puncture of the PCL (patients of the first group), type 1 blood supply allows you to safely make an alternative trans-parenchymal access directly to the lower calyx or pelvis through the inferior-lateral dorsal wall. The optimization of the access decreasesthe average operation time by 1.4 times and the average number of accesses by 1.3 times.
Conclusion. Doppler ultrasound scanning allows to visualize of arterial vessels, which helps to provide safe trans-cutaneous puncture access to PCS. In 73.2% of patients, the region of the posterior surface of the pelvis and the lower calyx was identified with the possibility of an anatomically justified low-traumatic trans-parenchymal access. It significantly expands the area of the parts of the PCS accessible for direct intervention. The creation of a trans-parenchymal access to the lower lateral parts of the renal pelvis allows reducing the total number of accesses to the PCS, which reduces the operation time and the number of complications.
For citations:
Malinin Yu.Yu. Alternative trans-parenchymal access for percutaneous contact nephrolithotripsy. Urology Herald. 2022;10(1):32-41. (In Russ.) https://doi.org/10.21886/2308-6424-2022-10-1-32-41
Introduction
Urolithiasis is one of the most widespread urological diseases. Its rate reaches 7–20% [1][2][3].
There are several options for surgical treatment of urolithiasis. Contact percutaneous nephrolithotripsy (PCNL) is a basic approach to the treatment of staghorn (coral) and large kidney stones [2][4][5]. Despite a long-term development period, one of the most important issues in endoscopic surgery is the creation of optimal access (or accesses) to a stone [2][5][6][7].
It is considered that percutaneous access should reach the pyelocalyceal system (PCS) along the shortest trajectory and go through the papilla of the small calyxes [5][7][8][9]. In the cases of multiple and (or) staghorn nephrolithiasis, access is made via a calyx that will allow for the removal of the main stone. It is also expected to provide multiple kidney fistulization (multiple access) and interventional cascading, which directly affects the rate of complications, surgery time, and general time of inpatient treatment [10].
Some authors believe it is necessary to make access along the lateral edge of the kidney in the avascular Zondek (Brödel) line, which is explained by the lack of major vessels in this area [7][9][11][12].
Anatomically, the kidney is divided into five relatively independent segments in terms of blood supply. The thickness of the posterior one is only a quarter of the kidney thickness, which allows assuming a significantly smaller number of vessels in this segment even outside the Zondek (Brödel) bloodless line. In most cases, the arterial blood supply to the upper, anterior, and lower segments of the kidney goes from the anterior pelvic branch of the renal artery, and the posterior segment is fed by a posterior pelvic branch of the renal artery. The posterior pelvic artery branch (posterior segmental artery) has a magistral structure and transverses the PCS posterior from the upper large calyx in 93% of cases and the posterior surface of the renal pelvis in 80% of cases [13]. At the same time, the data on the topographic anatomy of renal vessels remain controversial regarding the interaction within the vasculature of a kidney and its relation to the PCS [11][13][14].
In clinical practice, the relations between the arterial vasculature and PCS of the operated kidney are studied using computed tomography (CT) with virtual 3D modeling, selective arteriography, and color Doppler mapping (CDM). CDM can identify renal vessels around fistulization in real time and prevent damage during surgery, which reduces the rate of hemorrhagic complications [11][15].
The study aimed to evaluate the ultrasound anatomy of the renal vessels in the interventional interest area, i.e., its posterior and inferior segments and their association with PCS elements using CDM to provide grounds for alternative pathways of PCS fistulization.
Materials and methods
More than 10,000 transcutaneous surgeries for urolithiasis have been performed since 2000; 36% of them were for multiple and (or) staghorn (corral) stone kidneys.
The authors made a retrospective analysis of the treatment of 41 patients with urolithiasis who underwent PCNL and inpatient treatment in 2020 – 2021. Before surgery, patients were randomized into two groups comparable by sex, age, mean stone size, and forms of urolithiasis. Nine of them (22%) had multiple and 32 (78%) had staghorn nephrolithiasis.
The patients were examined according to the protocol standard for this category of patients: complaints, medical history, physical examination, clinical and instrumental studies, ultrasonic investigation, review and excretory urography, kidney CT, microbiological urine test, laboratory tests of the blood and urine. To verify the hypothesis on the possibility of creating alternative low-traumatic access to PCS before intervention and during fistulization, the authors performed CDM of the renal arteries using an Ultrasound Phillips HD7 scanner (Koninklijke Philips N.V., Philips Medical Systems Nederland B.V., Heerlen, The Netherlands) for arterial vessels and prevent their damage during PCNL.
The patients were distributed into two groups. Group 1 (study) contained 20 patients (48.8%) who had individual peculiarities of PCS anatomy (anterior orientation of lower calices), abnormal position and orientation of a kidney, peculiarities of the segmented intestine topography, or expressed meteorism. In these patients, traditional PCS fistulization access cannot be formed. Thus, PCS fistulization was achieved by transparenchymal access to the inferior lateral sections of the pelvis or the lower large calyx in the avascular area. Group 2 (control) contained 21 patients (51.2%). In this group, PCNL was performed in a standard approach (through the small calyx papilla). The ratio of men / women in Group 1 was 8/12, in Group 2 was 10/11. The age of the patients in the groups was comparable (24 to 72 years). The localization of stone(s) in the left / right side in Group 1 was 9/11, in Group 2, it was 10/11. The mean total size of the stone(s) liner in Group 1 was 3.7 cm, in Group 2 — 3.4 cm. Multiple stones were observed in 8 patients (40.0%) in Group 1 and 10 patients (47.6%) in Group 2. Staghorn nephrolithiasis was recorded in 12 patients (60.0%) in Group 1 and 11 patients (52.4%) in Group 2 (Table 1).
Table 1. Urolithiasis parameters
|
Estimated parameters |
Group 1 |
Group 2 |
|
Number of patients, n |
20 |
21 |
|
Localization (left / right) |
9/11 |
10/11 |
|
Average total linear stone size, cm |
3.7 (2.5–7.2) |
3.4 (2.6–7.0) |
|
Multiple PCS stones, n (%) |
8 (40.0%) |
10 (47.6%) |
|
Staghorn stones, n (%) |
12 (60.0%) |
11 (52.4%) |
Notes: PCS — pyelocalyceal system.
PCNL was performed in patients in the prone position using a rigid nephroscope 24–26 Ch Karl Storz MIP L (Karl Storz SE & Co. KG., Tuttlingen, Germany). In all cases, fistulization was made using Alken Telescopic Dilators. The stones were fragmented with an electro-impulse lithotripter Urolith (OOO MIT, Moscow Region, Balashikha, Russian Federation), ultrasonic lithotripter Karl Storz CALCUSIONÒ (Karl Storz SE & Co. KG., Tuttlingen, Germany), holmium laser lithotripter Karl Storz CALCULASEÒ II (Karl Storz SE & Co. KG., Tuttlingen, Germany), or their combination. All interventions were performed by one surgeon.
All patients signed informed consent for participation in the study.
Statistical analysis. Statistical analysis was performed with the MedCalc 18.10.2 software package (MedCalc Software Ltd., Ostend, Belgium). The analysis of intergroup differences between groups was performed with Student's T-test. The evaluation of the analyzed values was made with a calculation of the mean-square deviation. In all cases, the difference was statistically significant at p < 0.05.
Results
Regardless of the kidney side, CDM revealed that in 30 patients (73.2%), the blood supply around the standard access was going through the posterior segmental artery that passes posterior to the upper and middle PCS sections. Its branches are located above the collecting system of the lower group of calices and do not cross its inferior lateral dorsal projection to the parenchyma of the posterior kidney segment (type 1 blood supply) (Fig. 1).
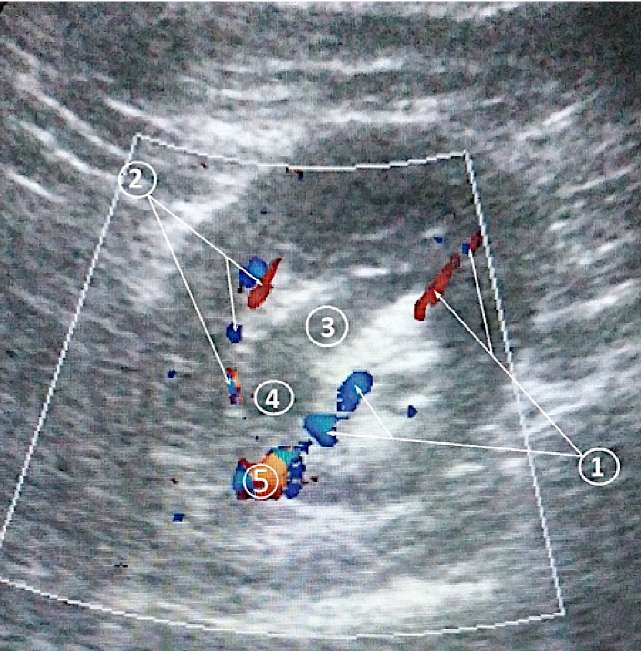
Figure 1. Dopplerogram of the left kidney of a patient with type 1 blood supply:
1. Arteries of the lower segment of the kidney. 2. Arteries of the posterior segment of the kidney.
3. Large renal calyx. 4. Renal pelvis. 5. Renal artery
In 11 patients (26.8%), the inferior branches of the posterior segmental artery that are responsible for the blood supply of the lower renal lobes and go posterior to the lower PCS sections (type 2) were around surgical interest.
In all patients from Group 1, CDM verified that there were no large arteries above the inferior lateral sections of the renal pelvis and the lower calyx during fistulization. This allowed posterior transparenchymal access to the PCS through the identified avascular zone outside small calyxes. The layout of the projection of the avascular area located between the posterior and inferior segments of the left kidney to the large calyx and renal pelvis is presented in Figure 2. The placement of trans-parenchymal pyelostoma allowed the surgeons to perform complicated stereoscopic manipulations on stones in a larger PCS area, and in some cases, remove all variously located stones via one access. Figure 3 shows a layout of possible vectors of PCS visualization (6 and 7) during transparenchymal The vectors of visualization 7 (red arrows) are possible only in the cases of the most medial accesses to the PCS.
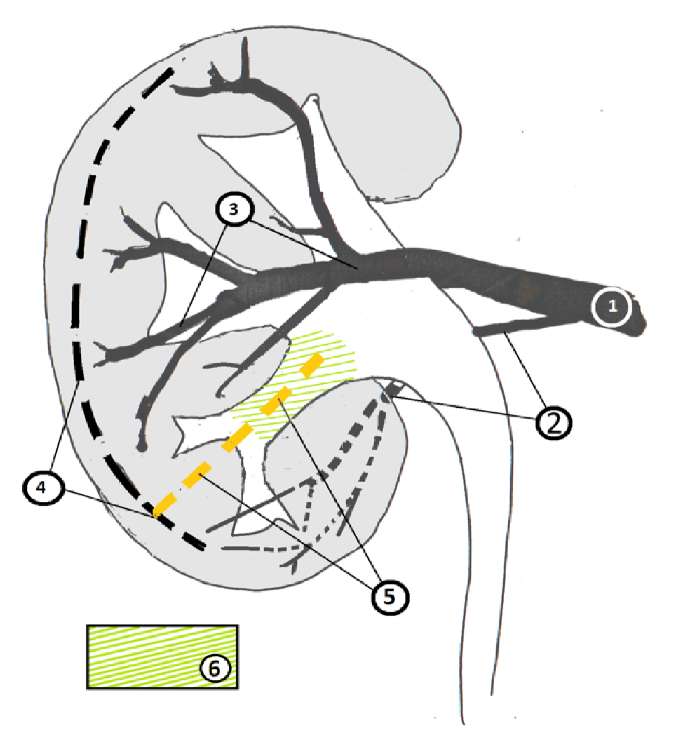
Figure 2. Scheme of the avascular zone projection located between the posterior
and lower segments of the left kidney onto the large calyx and pelvis in group 1 patients:
1. Renal artery. 2. Arteries of the inferior segment of the kidney.
3. Arteries of the posterior segment of the kidney.
4. Zondek (Brödel) line. 5. Avascular line.
6. Projection of the avascular zone on the pyelocalyceal system

Figure 3. Scheme of possible vectors for examining the pyelocalyceal system
during trans-parenchymal pyelostomy: 1. Renal artery.
2. Arteries of the inferior segment of the kidney.
3. Arteries of the posterior segment of the kidney. 4. Avascular line.
5. Projections of the avascular zone.
6 and 7. Scheme of possible pyelocalyceal system examination vectors
In three patients from the control group (14.3%), the punctured calyx was oriented dorsally and opened directly into the renal pelvis. Thus, it was possible to make standard access to a higher degree of stereoscopic freedom.
The authors made a comparative analysis of the following parameters between the two groups of patients: operation time, number of accesses, additional interventions, number of intraoperative and postoperative complications, and hospitalization time (Table 2).
Table 2. Intraoperative and postoperative characteristics
|
Indicators studied |
Group 1 |
Group 2 |
|
Average number of accesses, n |
1.2 ± 0.52 |
1.6 ± 0.75 |
|
Average time of the main stage of the operation, min |
40.6 ± 24.7 |
55.2 ± 27.2 |
|
Decreased hemoglobin level, g/l |
10.1 ± 4.8 |
14.2 ± 6.8 |
|
Blood transfusion, n (%) |
– |
1 (4.7%) |
|
Embolization of renal vessels, n (%) |
– |
1 (4.8%) |
|
Acute pyelonephritis, n (%) |
3 (15.0%) |
5 (23.8%) |
|
Re-operation to remove residual stones, n (%) |
3 (15.0%) |
4 (19.1%) |
|
Average hospitalization time, days |
7.6 ± 1.8 |
8.4 ± 1.6 |
|
Surgical treatment efficiency, % |
95.0 |
95.2 |
The average time of the main stage of the operation was 40.6 (15 – 95) minutes in Group 1 and 55.2 (20 – 135) minutes in Group 2. To specify the volumetric characteristics of blood loss, the authors studied a decrease in hemoglobin level on day 2 after the intervention. In Group 1, it was 10.0 ± 4.8 g/L and 14.2 ± 6.8 g/L in Group 2. The average number of bed-days was 7.6 days in Group 1 and 8.4 days in Group 2. The average number of accesses per patient was 1.2 (max 2) in Group 1 and 1.6 (max 3) in Group 2. Repeated surgery for the removal of the residual stones was required in three patients (15%) from Group 1 and four patients (19.1%) from Group 2. Postoperative acute pyelonephritis was observed in three (15%) patients from Group 1 and five (23.8%) patients from Group 2. A blood transfusion with additional embolization of the fornical artery was performed in a patient (4.8%) of Group 2. The summed effectiveness of the performed surgical treatment showed that there was not much difference between the groups (95.0% versus 95.2%).
In Group 1, there was a decrease in the average time of surgery by 1.4 times, the average number of accesses by 1.3 times, and a slight reduction of hospitalization time.
DISCUSSION
The avascular Zondek (Brödel) line is found along the posterior surface of the kidney and acts as an interspace in the parenchyma between the pools of blood supply from the posterior (posterior segment) and anterior segmental arteries (superior, anterior, and inferior segments). In other words, it is a line of natural division of the The creation of PCS access through this avascular region of the parenchyma is most favorable due to the low probability of large arterial vessel damage [7][9][11][12]. Due to the peculiarities of the arterial blood supply, anatomically, the kidney is divided into five independent segments. The lower segment has ventral and dorsal surfaces. In the case of the anterior pelvic orientation of the inferior segmental artery, there is an anterior-posterior direction of the arterial blood flow and no branches of the posterior segmental artery in the lower segment of a kidney. The published data on the topography of the renal arteries are incomplete and sometimes appear controversial concerning the segmental arteries and their relation to PCS [11][14]. Thus, they can be characterized by a variable topography. The results of the study showed that in a quarter of cases, the dorsal segments of the lower pole of a kidney were blood supplied through the posterior segmental artery system (type 2 blood supply). On the one hand, it contradicts the canonic picture of the character of a segmented division of a kidney. On the other hand, it rejects a hypothesis on a low significance of blood vessels in the pool of the posterior segmental artery for the blood supply around the expected surgical interest (Fig. 4).
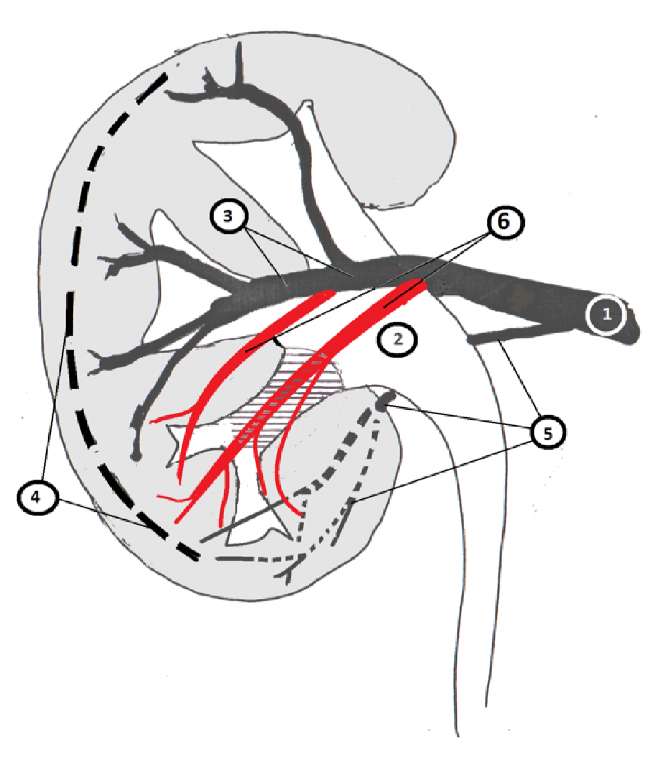
Figure 4. Scheme of the possible location of the branches
of the posterior segmental artery in patients with type 2 blood supply:
1. Renal artery. 2. Renal pelvis. 3. Arteries of the posterior segment of the kidney.
4. Zondek (Brödel) line. 5. Arteries of the inferior segment of the kidney.
6. Branches of the posterior segmental artery duplicate the lower segmental arteries
On the one hand, the study results showed that in 73.2% of patients, the arterial blood supply of the lower segment of a kidney corresponded to the generally accepted division of a kidney into segments. Posterior segmental arteries go above the lower group of calices and do not transverse the projection of the lower calyx and the inferior lateral dorsal projection of the renal pelvis onto the renal parenchyma. The branches of the inferior segmental artery go inferior and anterior to the specified PCS structures, which means that it is possible to create trans-parenchymal access to the lower calyx or posterior lateral sections of the renal pelvis. It will go through the avascular area, which does not contradict the published data [15]. To sum up, it can be suggested that the avascular area, revealed by the authors, is an anatomic analog of the Zondek (Brödel) line and a natural border between the posterior and lower segments of the kidney.
The inconveniences that arise during the creation of classic access to the PSC make researchers search for alternative pathways of fistulization that may differ from conventional ones. Thus, there are publications on the possibility of extrapapillary fistulization that show the feasibility of accessing the small calyx near the papilla, and possible complications that develop after the arcade and interlobular vessels damage are considered insignificant [16][17]. On the other hand, some authors believe that transcutaneous nephrostomy performed through the small calyx neck is dangerous because it leads to a significant risk of hemorrhage from the fornical vessels. Besides, an unsuccessful puncture of the large calyx renal calyx and its neck leads to a risk of bilateral puncture of the PCS and damage of the associated arteries [18].
The available publications show that endoscopic intervention through the pyelostoma is prohibited, which can be associated with such technical peculiarities of this access as easily changing geometric parameters of the renal pelvis, its relatively thin wall (that may lead to a possible loss of the pyelostomy channel), difficulties in nephrostomy for drainage and hemostatic purposes, the possibility of damaging large and magistral vessels, etc. Surgeons do not consider the possibility of transparenchymal access to the lateral lower sections of the PCS. The presence of an avascular area at the site of contact of the vascular system of the lower, lower anterior, and posterior segments provides safe alternative accesses to the PCS with a larger area of punctured parenchyma.
Fistulization through the avascular area avoids the mentioned drawbacks. Fistulization that is more medial than standard reduces geometrical limitations of standard accesses, creating conditions for stereoscopically more complicated manipulations with stones in the PCS even when rigid tools are used and decreasing the number of accesses required for stone removal.
It should be highlighted that the renal arterial system has a very individual character. Therefore, it is necessary to consider the possibility of a physiological linear shift in the boundaries between the lower and posterior segments of the kidney in the inferior-superior and anterior-posterior directions, as well as various anatomical and vascular aberrations. The last suggestion is confirmed by the results of the study obtained. The application of CDM during puncture provides safe transparenchymal access.
It can be suggested that the success of the alternative PCS access applied during the study, except for the puncture through the avascular area, is explained by the following factors. First, it can be explained by the expressed changes in the PCS size caused by nephrolithiasis. Second, the applied retrograde contrast of PCS caused pyelocalicoectasia within the physiological limits. Third, the application of Alken telescopic dilators to crease the access allowed surgeons to avoid PCS detachment from the renal parenchyma even when a large-diameter nephroscope was used. Therefore, Karl Storz nephroscopes were used due to the peculiarities of their irrigation system.
The implementation of an alternative transparenchymal access to PCS can stimulate further development of rigid minipercutaneous and macropercutaneous lithotripsy in the therapy of multiple kidney stones by reducing the necessity for the application of flexible renoscopy. When it is implemented in surgical routine practice, it will significantly reduce the cost of the treatment.
CONCLUSION
- Ultrasonic Doppler scanning provides visualization of arterial vessels that are important for the creation of free transcutaneous puncture access to the PCS.
- In 73.2% of patients, there is an area in the posterior surface of a renal pelvis and lower large calyx that can provide low-traumatic transparenchymal access, which can significantly expand the area of PCS sections available for direct intervention.
- Transparenchymal access to the lower lateral renal pelvis sections decreases the average number of accesses to the PCS, which reduces the time of surgery and rate of complications.
References
1. López M, Hoppe B. History, epidemiology and regional diversities of urolithiasis. Pediatr Nephrol. 2010;25(1):49-59. DOI: 10.1007/s00467-008-0960-5.
2. Trusov P.V., Kogan M.I., Khvan V.K. The efficacy and safety of mini-percutaneous nephrolithotripsy in the treatment of large and staghorn stones of the kidney. Vestnik Urologii. 2017;5(1):32-36. (In Russ.). DOI: 10.21886/2308-6424-2017-5-1-32-36.
3. Seitz C, Fajkovic H. Epidemiological gender-specific aspects in urolithiasis. World J Urol. 2013;31(5):1087-92. DOI: 10.1007/s00345-013-1140-1.
4. Preminger GM, Assimos DG, Lingeman JE, Nakada SY, Pearle MS, Wolf JS Jr; AUA Nephrolithiasis Guideline Panel). Chapter 1: AUA guideline on management of staghorn calculi: diagnosis and treatment recommendations. J Urol. 2005;173(6):1991-2000. DOI: 10.1097/01.ju.0000161171.67806.2a.
5. Kogan M.I., Akilov F.A., Martov A.G., Dutov V.V., Grigor'ev N.A., eds. Innovacionnaya hirurgiya kamnej pochek i mochetochnikov. Moscow: Medkongress; 2021. (In Russ.). ISBN 978-5-6045500-1-4.
6. Lahme S. Miniaturisation of PCNL. Urolithiasis. 2018;46(1):99-106. DOI: 10.1007/s00240-017-1029-3.
7. Alken P. Percutaneous nephrolithotomy - the puncture. BJU Int. 2022;129(1):17-24. DOI: 10.1111/bju.15564.
8. Yu W, Ruan Y, Xiong Z, Zhang Y, Rao T, Cheng F. The Outcomes of Minimally Invasive Percutaneous Nephrolithotomy with Different Access Sizes for the Single Renal Stone ≤25 mm: A Randomized Prospective Study. Urol Int. 2021:1-6. DOI: 10.1159/000516914. Epub ahead of print. PMID: 34198290.
9. Kolsanov AV, Murushidi MYu, Korolev DG. Methods for navigating access to the kidney in percutaneous nephrolitholapaxy. Russian Journal of Operative Surgery and Clinical Anatomy. 2020;4(3):37-43. (In Russ.). DOI: 10.17116/operhirurg2020403137.
10. Trusov P.V., Gusev A.A. Treatment of kidney stones: standards and innovations. Vestnik Urologii. 2019;7(2):93-111. (In Russ.). DOI: 10.21886/2308-6424-2019-7-2-93-111.
11. Macchi V, Picardi E, Inferrera A, Porzionato A, Crestani A, Novara G, De Caro R, Ficarra V. Anatomic and Radiologic Study of Renal Avascular Plane (Brödel's Line) and Its Potential Relevance on Percutaneous and Surgical Approaches to the Kidney. J Endourol. 2018;32(2):154-159. DOI: 10.1089/end.2017.0689.
12. Sharma GR, Maheshwari PN, Sharma AG, Maheshwari RP, Heda RS, Maheshwari SP. Fluoroscopy guided percutaneous renal access in prone position. World J Clin Cases. 2015;3(3):245-64. DOI: 10.12998/wjcc.v3.i3.245.
13. Bouzouita A, Saadi A, Hermi A, Chakroun M, Bouchiba N, Allouche M, Hamdoun M, Mighri MM, Chebil M. Cadaveric study of arterial renal anatomy and its surgical implications in partial nephrectomy. Surg Radiol Anat. 2021;43(9):1449-1459. DOI: 10.1007/s00276-021-02769-8.
14. Klatte T, Ficarra V, Gratzke C, Kaouk J, Kutikov A, Macchi V, Mottrie A, Porpiglia F, Porter J, Rogers CG, Russo P, Thompson RH, Uzzo RG, Wood CG, Gill IS. A Literature Review of Renal Surgical Anatomy and Surgical Strategies for Partial Nephrectomy. Eur Urol. 2015;68(6):980-92. DOI: 10.1016/j.eururo.2015.04.010.
15. Lu MH, Pu XY, Gao X, Zhou XF, Qiu JG, Si-Tu J. A comparative study of clinical value of single B-mode ultrasound guidance and B-mode combined with color doppler ultrasound guidance in mini-invasive percutaneous nephrolithotomy to decrease hemorrhagic complications. Urology. 2010;76(4):815-20. DOI: 10.1016/j.urology.2009.08.091.
16. Kallidonis P, Vagionis A, Lattarulo M, Adamou C, Tsaturyan A, Liourdi D, Vrettos T, Simeone C, Liatsikos E. Non-papillary percutaneous nephrolithotomy for treatment of staghorn stones. Minerva Urol Nephrol. 2021;73(5):649-654. DOI: 10.23736/S2724-6051.20.04124-7.
17. Kallidonis P, Vagionis A, Vrettos T, Adamou K, Pagonis K, Ntasiotis P, Callas GA, Tanaseskou L, Al Aown AM, Liatsikos E. Non papillary mini-percutaneous nephrolithotomy: early experience. World J Urol. 2021;39(4):1241-1246. DOI: 10.1007/s00345-020-03267-z.
18. Kolsanov AV, Nazaryan AK, Yaremin BI, Ivanova VD, Yunusov RR. 3D imaging in the study of the variant anatomy of renal arteries. Russian Journal of Operative Surgery and Clinical Anatomy. 2017;1(1):44-48. (In Russ.). DOI: 10.17116/operhirurg20171144-48.
19. Francisco J.B. Surgical Anatomy of the Kidney for Endourological Procedures. In: Smith AD, Preminger GM, Kavoussi LR, Badlani GH, FACS, FRCS (Hon), Rastinehad AR, FACOS, eds. SampaioSmith's Textbook of Endourology. DOI: 10.1002/9781119245193.ch6.
About the Author
Yu. Yu. MalininRussian Federation
Yury Yu .Malinin — M.D., Cand.Sc.(Med); Head, Dept. of Urology
Donetsk, DPR
Review
For citations:
Malinin Yu.Yu. Alternative trans-parenchymal access for percutaneous contact nephrolithotripsy. Urology Herald. 2022;10(1):32-41. (In Russ.) https://doi.org/10.21886/2308-6424-2022-10-1-32-41













































