Scroll to:
Global Secular Trend of Gonadal Size in Men: Review and Analysis of Publications
https://doi.org/10.21886/2308-6424-2029-8-1-75-91
Abstract
Introduction. Notwithstanding the general increase in world population, there is a steady decline in birth rate. Studies have shown a tendency towards worsening of qualitative and quantitative indices of the ejaculate. From the foregoing we may also presume a decline in size of male gonads. Nevertheless, information about the tendency of change in testicular size in the population is currently unavailable.
Purpose of the study. Assessment of global secular trend as regards changes in the size of testes in men.
Materials and methods. A search was conducted on published scientific research in the English language and Russian language in Pubmed and eLibrary. Additional searches in citations of identifiable investigations. A selection of data from publications with metric characteristics of gonads in relatively healthy men aged 18‒60 years. The mean of values obtained were determined and homogenized with the aid of formulae for volume calculations. Statistical analysis of the data was carried out with the aid of the program STATISTICA for Windows v.10.
Results. The search yielded 126 identified publications, published between 1902 and 2018. Analysis of the various works led to a selection of 33, which contained information that satisfied the inclusion criteria. Analysis of the obtained data did not reveal any trends in change of testicular size over the past century. Mean arithmetic weighted value was 17,43±5,64; 95% CI (17,32; 17,54).
Conclusion. In the light of global trends towards a reduction in fertility, it is necessary to conduct a wide range of varied investigations in order to understand the nature of this process. Standardization of methods of assessment results obtained will help in reducing errors whilst assisting in the analysis of existing tendencies.
For citations:
Seroukhov A.Yu., Afoko A.A., Mamaev I.E. Global Secular Trend of Gonadal Size in Men: Review and Analysis of Publications. Urology Herald. 2020;8(1):75-91. https://doi.org/10.21886/2308-6424-2029-8-1-75-91
Introduction
Reproductive health is one of the goals for the development humankind adopted by the General Assembly of the UN in 1994. Despite general increase in the population of the world, there has been a steady decline in fertility in the last decades [1, 2] (Figure 1). It must be noted that this problem is linked to the increase in several infertile couples worldwide.
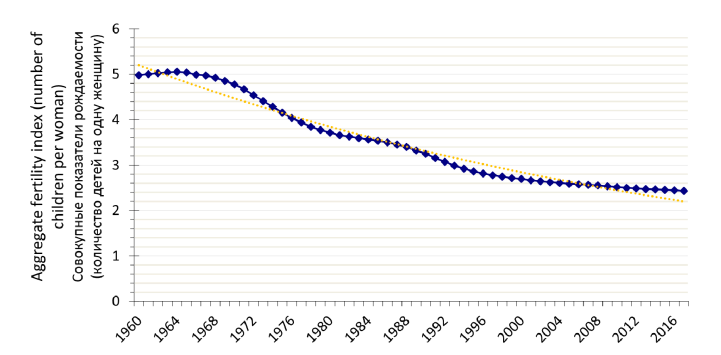
Figure 1. Aggregate indices of fertility (number of births per woman) worldwide, 1960-2017 years [3]
Рисунок 1. Совокупные показатели рождаемости (число рождений на одну женщину) во всем мире, 1960-2017 годы [3]
Most research studies indicate that 15% of couples remain infertile after 1 year of attempting to conceive a child [4-6]. This information is based on the WHO report published in 1991 [7], as well as a row of other studies carried out over two past decades [8, 9]. Considering the global tendency towards a reduction in fertility, it is possible that currently, the percentage of couples without children is higher than recognized above. Concerning gender, the male factor of infertility accounts for a little over 50% [10]. The ability of a man to impregnate a woman is closely related to the qualitative and quantitative characteristics of the ejaculate. Currently, the WHO has established a lower level of normal sperm concentration to 15*106/ml [11]. Nonetheless, many authors concede that for normal fertility this parameter should be 40*106/ml or higher [12-14]. The majority of studies in the first half of the 20th Century noted a rather high concentration of spermatozoa in the ejaculate of healthy men. On the average, this was about 100*106/ml [15, 16]. In 1992, results of a meta-analysis were published for semen analysis of healthy men. The authors included the period from the 1930s to the 1990s of the previous century. From the results of the above, it was established that there is a global tendency towards the worsening of sperm quality (Figure 2) [16]. The initial results appeared doubtful, but after scrutiny and verification and taking into account geographical considerations among others, the results were found to be comparable. The observed reduction in the concentration of sperm of men in North America is about 1.5% per year and in Europe about 3.1% [17, 18]. According to data from contemporary population series, the sperm concentration in healthy men varies according to a geographical location but on the average ranges between 41-63*106/ml [19-23].
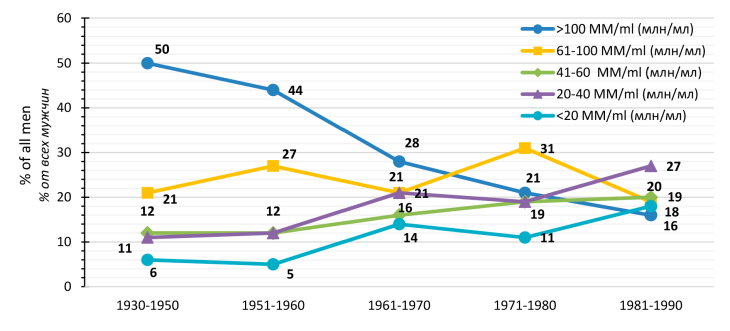
Figure 2. Percentage proportion of men with different ranges of sperm concentration in different periods of investigations (data from 27 publications). From Carlsen et al.,1992 [16]
Рисунок 2. Процентное соотношение мужчин с различными диапазонами концентрации сперматозоидов в разные годы исследований (данные из 27 публикаций). Из Carlsen с соавт.,1992 [16]
It is important to note that the concentration of spermatozoa in the ejaculate is directly related to the size of the testis [24-28]. From the above information, one may propose the presence of a negative dynamic in testicular size. However, information about the trends in change of testicular size in the population is absent. The non-uniformity of methods for measurement of testicular volume [29] and lack of standardization in the latter process leads to a wide variation of current data, thereby making retrospective analysis of the given parameter rather difficult.
Purpose of the study. The objectives of the current study are to evaluate the global secular trend in the change in the size of testes in men.
Materials and methods
We searched for studies in English and Russia languages that assessed testicular size. For this purpose, we employed resources from Pubmed and eLibrary. Also, we analyzed citations from the literature obtained, with subsequent inclusion of the same in the selection after satisfying the given criteria. We did not set limits about the date of publication. From this volume of information, we selected data related to testicular size in men aged between 18-60 years. We excluded studies whose subjects were selected based on fertility or the presence of disease conditions such as varicoceles or cryptorchidism, that have the potential to affect testicular volume. From cadaveric studies, we excluded those that assessed volume or weight without removal of the epididymis or those which had no information about the extent of dissection of the specimens. Apart from that, in our review, we did not include studies in which only one linear dimension of the testis was measured, as well as those that employed Hynie orchidometer [30]. The next stage involved the homogenization of the various methods of measurement and calculation of the mean volume, the closest to the actual values.
For this purpose, we used the following formulae for the determination of the volume (V):
(1) V=m/1.038
where m — a mass of the organ; 1.038 — density.
(2) V=a*b*c*0.71
where a, b, c — corresponding length, width and height; 0.71 — Lambert's coefficient.
(3) V=a*b2*0.71
where a, b — corresponding length and width; 0.71 — Lambert's coefficient.
(4) V=V1/0.52*0.71
where V1 — volume calculated using the ellipsoid or prolate spheroid formula; 0.52 — coefficient for ellipsoid or prolate spheroid formula; 0.71 — Lambert's coefficient.
(5) V=a*b2*0.39
where a, b — corresponding length and width, calculated by means of external measurements without taking skin into the account; 0.39 — correction coefficient.
(6) V=VPr*0.816
where VPr — volume obtained with the aid of Prader orchidometer or similar meter; 0.816 — correction coefficient.
(7) V=VTh/0.52*0.39
where VTh — volume obtained with the aid of Takihara orchidometer; 0.52 — coefficient for ellipsoid or prolate spheroid formula; 0.39 — correction coefficient.
(8) V=V1K/0.71*0.39
where V1K — volume obtained with the aid of
Lambert's formula, using external measurement without consideration of the thickness of skin; 0.71 — Lambert's coefficient; 0.39 — correction coefficient.
Statistical analysis of the data was carried out with the aid of the program STATISTICA for Windows v.10. For the assessment of the size of the gonads in adult males, a time series was constructed. A calculation of mean base and chain-growth rate, as well as a rate of increment, was carried out. The method of enlarging the intervals was utilized (a calculation of mean arithmetic levels of a given period). A calculation of the moving average -mean arithmetic for 3 and 5 years (calculated intervals cross each other), we carried out time series smoothing by 3 and 5 point averages, also we cross-checked the dynamic rows for the presence of any trends with the aid of linear and power functions.
Results
We identified 126 studies following the search carried out, which were published between 1902 and 2018. Further analysis of the publications led to a selection of 33, in which the information contained therein satisfied our set criteria for selection (Table 1). The period of these selected articles ranged from 1902 to 2016. The total number of men involved in the selected studies was 11932. From the selected studies, based on the method of determination of testicular size, we got the following distribution: 8 (24.24%) — assessment was on autopsy specimens by means of weighing or displacement of water, 4 (12.12%) — determination of linear dimensions, also of cadaveric material, 6 (18.18%) — the use of external linear measurements in living subjects, 7 (21.21%) — determination by means of Prader (6) or Takihara (1) orchidometer and 8(24.24%) — by use of ultrasonography (Figure 3).
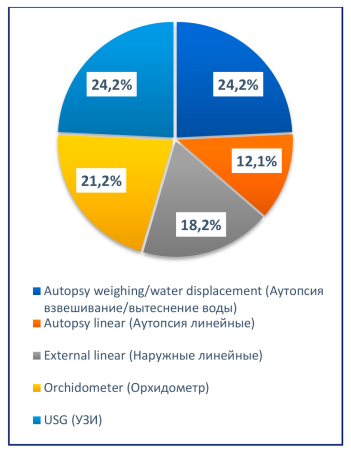
Figure 3. Distribution of studies based on the method of measurement
Рисунок 3. Распределение работ по методам измерения
Table 1. Investigations of the gonadas size in adult males
Таблица 1. Исследования размера наружных половых желез у взрослых мужчин
Author Автор | Year Год | Country of investigation Страна проведения исследования | Number of objects (n) Количество объектов (n) | Age (years) Возраст (лет) | Method of measurement Метод измерения | Dimension Размер | Mean calculated volume (cm3) Усреднённый вычисленный объём (см3) | ||||||||||
1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | ||||||||||
Spangaro a | 1902 | Germany Германия | 10 | 19-45 | Linear Autopsy Линейные Аутопсия | 45х30х23,5 mm (мм) | V=a*b*c*0,71= 22,53 | ||||||||||
Shultze a | 1913 | Germany Германия | No data Нет данных | ≥18 | Linear Autopsy Линейные Аутопсия | 42,5x27,5x21 mm (мм) | V=a*b*c*0,71=17,43 | ||||||||||
Mita a | 1914 | Germany Германия | No data Нет данных | ≥18 | Linear Autopsy Линейные Аутопсия | 38x24x23 mm (мм) | V=a*b*c*0,71=14,89 | ||||||||||
Romeis a | 1926 | Germany Германия | No data Нет данных | ≥18 | Weighing Autopsy Взвешивание Аутопсия | 19,6 g (г) | V=m/1,038=18,88 | ||||||||||
Roessle and Roulet a | 1932 | Germany Германия | >500 | 21-60 | Weighing Autopsy Взвешивание Аутопсия | 17,75 g (г) | V=m/1,038=17,1 | ||||||||||
Peter et al. a'e | 1938 | Germany Германия | No data Нет данных | 19-45 | Weighing Autopsy Взвешивание Аутопсия | 18 g (г) | V=m/1,038=17,34 | ||||||||||
Schonfeld and Beebe [31] | 1942 | USA США | 125 | 18-25 | Orchidometer "Prader" Орхидометр "Prader" | 16,27 ml (мл) | V=V Pr*0,816=13,28 | ||||||||||
Olesen c'd | 1948 | Denmark Дания | 140 | ≥18 | Weighing Autopsy Взвешивание Аутопсия | 21 g (г) | V=m/1,038=20,23 | ||||||||||
Hansen b | 1949 | Denmark Дания | 33 | ≥18 | Linear. Ellipsoid formula (minus skin) Линейные Формула Эллипсоида (минус кожа) | 11,75 cm3 (см3) | V=V1/0,52*0,71=16,04 | ||||||||||
Lambert [32] | 1951 | Sweden Швеция | 54 | 42 | Linear. Lambert's formula (minus skin) Линейные Формула Lambert (минус кожа) | 20,8 cm3 (см3) | V=20,8 | ||||||||||
Hansen and Torben [33] | 1952 | Denmark Дания | 844 | ≥20 | Linear. Lambert's formula (minus skin) Линейные Формула Lambert (минус кожа) | 17,35 cm3 (см3) | V= 17,35 | ||||||||||
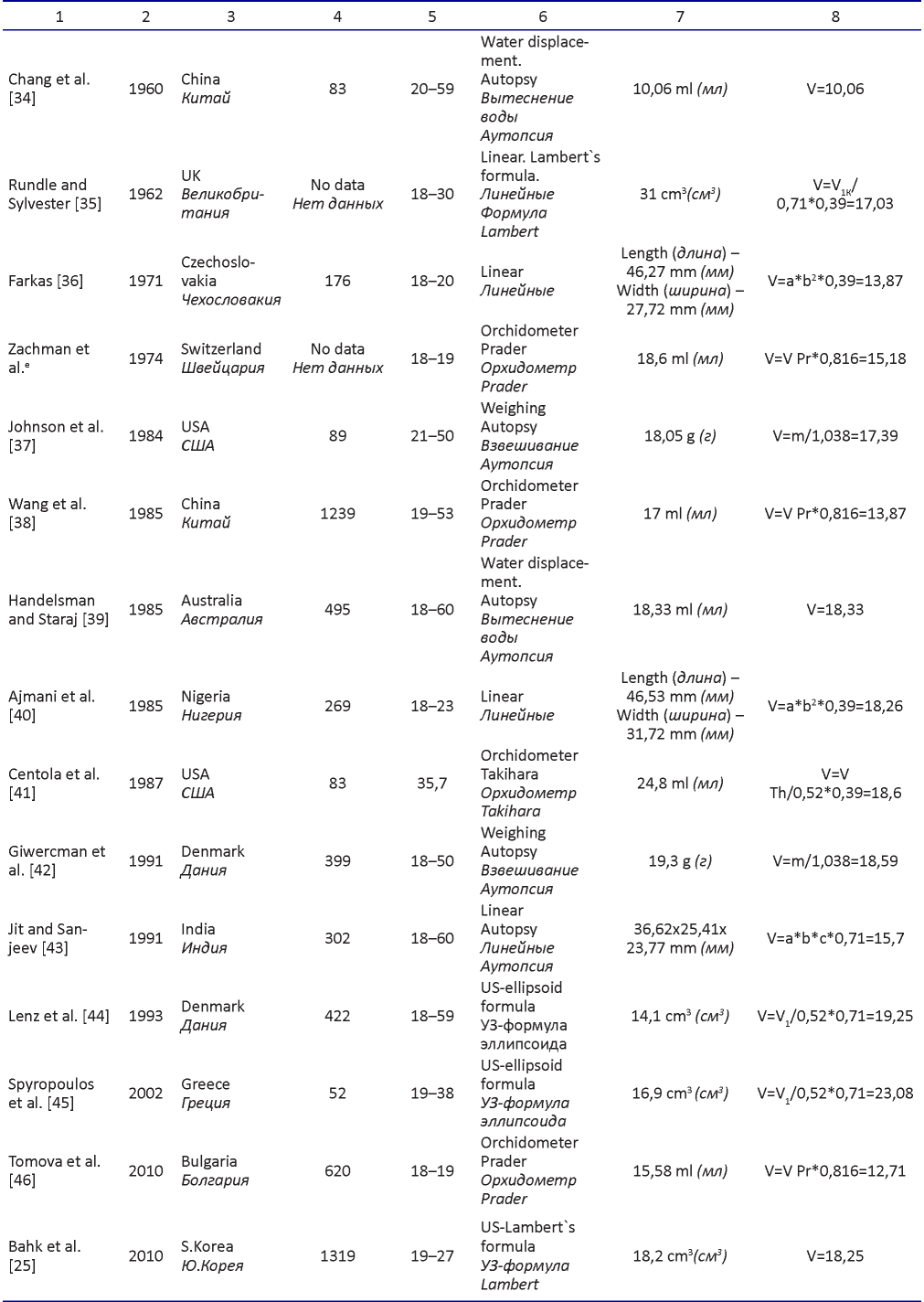
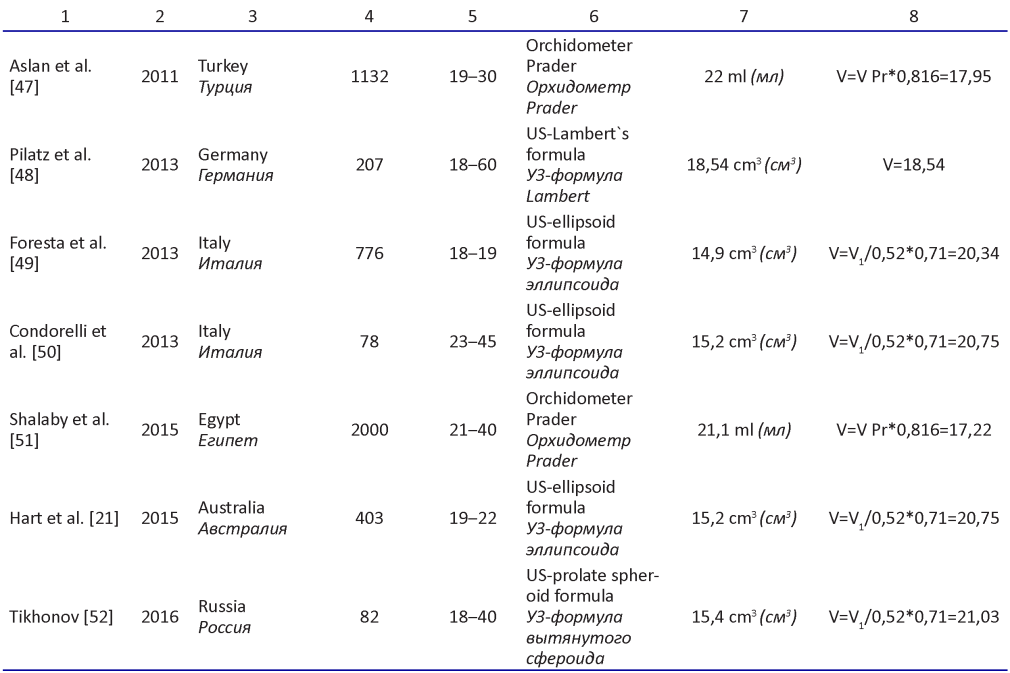
Comment: a from Lambert,1951; b from Hansen, 1952; c from Short, 1984; d from Giwercman ,1991; e from Jit, 1991
Примечания: a из Lambert, 1951; b из Hansen, 1952; c из Short, 1984; d из Giwercman, 1991; e из Jit, 1991
According to the results of the calculations with the aid of the standardizing formulae, we found the calculated mean volume of each study (Figure 4). After statistical analysis of the data, the weighted arithmetic mean value was 17.43±5.64; 95% CI (17.32, 17.54). The coefficient of variation obtained was 32.34%, and this confirms the uniformity of the sizes within the period under investigation. Therefore, based on the data obtained, there were no statistically significant tendencies observed in the change of volume of testes for the last century.
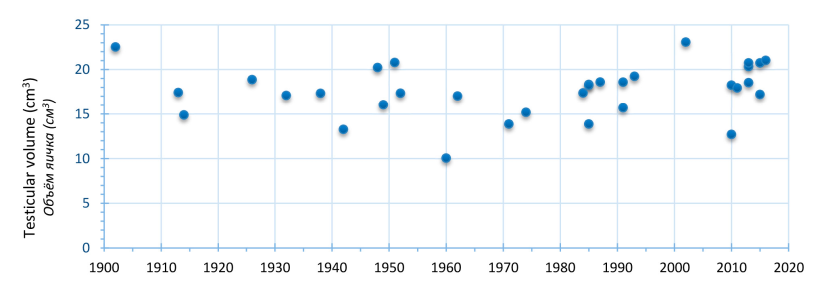
Figure 4. Homogenized results of investigations of the volume of the testes over time in years
Рисунок 4. Гомогенизированные результаты исследований объёма яичка по годам
Discussion
Testicular volume in adults is mainly determined by the pool of differentiating germ cells as well as Sertoli cells. Many studies have established a direct quantitative relationship between the abovementioned components of the testes and the outcome of germ cells. Considering the tendency worldwide of a reduction in the concentration of spermatozoa, it would have been logical to expect a similar tendency of reduction in testicular volume. As far as we know, such findings at present are absent.
Giwercman et al. (1991) made such an assumption. However, when they compared results from cadaveric studies from Olesen (1948), which were done at the same facility 40 years earlier, there was no statistically significant reduction in testicular size [42].
Carrying out of retrospective analysis is problematic for a couple of reasons. The main problem lies in the fact that there is no standardization of the methods employed in measuring testicular dimensions. Earlier studies were based often on the assessment of cadaveric material. The authors seldom commented on the extent of dissection of the testes, often weighed the specimens with the epididymis (Spangaro,1902; Stieve,1930 from Lambert,1951[32]). Part of dimensional studies were carried out after fixation of the specimens [53].
As recently as the 1970s, in clinical practice, the testicular size was compared to different objects of similar shape (peas, beans, grapes, hazelnuts), or subjectively characterized by authors as "small- normal" [29].
In 1942 Schonfeld and Beebe were the first to invent an orchidometer, which consisted of 23 ellipsoid models of known volume. Comparison of the testis during palpation with the model of similar size allowed for estimation of testicular volume [31]. The Prader orchidometer, which was proposed in 1966 and became popular, remaining widely in use up to date, was based on the same principle [54]. Its simplicity and low cost popularized the method among researchers and clinicians alike. A series of comparative volumetric studies indicated that a high correlation of volume between the estimated and actual. This notwithstanding, the estimated volumes were found eventually to be higher, besides, there were high reproducibility errors inherent in the process of measurement [55-62].
External measurements with the aid of a ruler or callipers were also actively employed for the evaluation of testicular size [32, 33, 35, 40, 63-70]. In the event of direct measurement of testicular size with the aid of rulers, an unavoidable error arises as a result of the inclusion of the skin and testicular tunics. Therefore, some authors suggested the subtraction of the duplication of the scrotal skin from the results of such measurements [32, 33].
The Hynie orchidometer [30] was quite popular and widely used among clinicians. The basis for calculation for this device lies in the measurement of the length of the testis (it's longest dimension-d) and applying this in the formula V=d3/4 to determine the volume of the testis [29]. It was quite predictable that comparative volumetric investigations will reveal wide margins of error using this device [55]. Another type of orchidometer was introduced by Takihara in 1983. This device consists of stencil ellipsoid rings of different sizes. The corresponding size to the testis was slipped over the gonad with the scrotal skin stretched. The calculation of the volume using this device is based on the formula of a prolate spheroid: V=0.52*a*b2 [71].
In contemporary research as well as in current clinical practise, we often employ ultrasonography for the assessment of testicular volume. This method allows us to determine more accurate dimensions due to clear visualization. However, just as with the external linear measurements, there was no consensus on the most appropriate formula for calculating the volume. Most often we employ already installed formulae on the ultrasound machines for calculating the volume of an ellipsoid: (V=0.52*a*b*c) or that of a prolate spheroid: (V=0.52*a*b2) [48]. In recently published recommendations, the working group of the European Society of Urogenital Radiology agreed to use Lambert's formula (V=0.71*a*b*c), in computing the volume of the testis during ultrasound investigations, as the closest in correlation to the actual testicular volume [72].
Another important factor that makes retrospective analysis difficult to carry out is the fact that testicular size varies greatly among different age groups. Most contemporary studies focus on the measurement of testicular volume in children and adolescents as a factor of sexual development [46, 61, 62, 66, 67, 69, 73-91]. The size of gonads after puberty alters only insignificantly. Testicular volume will tend to reduce only after 60 years of age [48, 53, 92-95].
Most often researches focus their investigations on certain disease states of the male reproductive system which have the potential to affect the size of the gonads. This may be a selection based on fertility [28, 96, -100], the presence or absence of a varicocele [41, 81, 99, 101, 102], cryptorchidism in the past medical history [68, 103] or indeed from andrological patients [26, 60].
Finally, some researches point to the fact that there are racial and ethnic differences in the size of gonads in adult males [71, 79, 104].
In the current study, we analyzed the volume of the testes in healthy men aged 18-60 years using available publications in the literature. After the selection of data that satisfied the required criteria, we homogenized the given volumes. The measurement of testicular volume based on the Archimedes principle of displacement of water was considered the most accurate. The density of the testis without the epididymis is 1.038 g/cm3 [94]. This parameter was used to calculate the volume in the studies that were carried out through a measurement of the mass of the testis (Formula 1).
Even though the shape of the testis is like a prolate spheroid, many studies indicate that more accurate results can be obtained using Lambert's formula with a coefficient of 0.71[32, 55, 59, 105, 106]. For this reason, we used Lambert's formula for calculation of testicular volume, whose linear dimensions are known (Formula 2 and 3).
In his original article, Lambert pointed out the importance of subtracting the skin thickness when calculating testicular volume with the aid of external linear measurements [32]. In studies where the authors subtracted the skin thickness but then calculated the testicular volume using the formula of an ellipsoid, we recalculated by employing Lambert's coefficient (Formula 4).
V. Dornberger and G. Dornberger [55] in their studies based on comparative volumetric investigations suggested a correction coefficient of 0.39 in the ellipsoid formula during external measurements which were carried out without taking into account the thickness of the skin. We utilized this in formula 5. In the case where the authors calculated the volume of the testis using Lambert's formula without subtracting the skin thickness, we employed formula 8. The principle behind the Takihara orchidometer is based on the ellipsoid formula. The idea behind this method is similar to that of external linear measurements without correction for skin thickness. For the determination of testicular volume in such cases we employed formula 7.
The margin of error with the use of the Prader orchidometer varies widely depending on the age and volume of the testis [61, 85]. For volume calculation, we used the adjusted coefficient of 0.816 which was suggested by Sakamoto [59] (formula 6).
Ultrasound results were recalculated using Lambert's formula.
Analysis of the data we obtained confirms the absence of any kind of significant global secular trends in the testicular size of adult males. This does not correlate with the concept of a global tendency towards a reduction of sperm concentration in the ejaculate.
There is a possibility that the factors which have an inhibitory action on spermatogenesis, do not necessarily lead to a reduction in the number of Sertoli and germ cells, i.e. the weight and volume of the testis, but influences the differentiation of the latter.
Conclusion
In the light of global trends towards reduction infertility, it is necessary to carry out further wideranging investigations in order to elucidate the nature of the process. Standardization of methods of assessment of the results will aid in reducing the margins of error and this will assist in the analysis of the existing tendencies.
References
1. United Nations, Department of Economic and Social Affairs, Population Division. The World Population Situation in 2014 A Concise Report. (ST/ESA/SER.A/354) 2014. Available at: https://www.un.org/en/development/desa/population/publications/pdf/trends/Concise%20Report%20on%20the%20World%20Population%20Situation%202014/en.pdf Accessed November 25, 2019
2. United Nations, Department of Economic and Social Affairs, Population Division. World Fertility Patterns 2015. Data Booklet (ST/ESA/SERA/370) 2015. Available at: https://www.un.org/en/development/desa/population/publications/pdf/fertility/world-fertility-patterns-2015.pdf Accessed November 25, 2019
3. World Bank, World Development Indicators. Fertility rate, total (births per woman) 2019. Available at: https://data.worldbank.org/indicator/SP.DYN.TFRT.IN AccessedNovember 25, 2019
4. Meacham RB, Joyce GF, Wise M, Kparker A, Niederberger C. Male Infertility. Journal of Urology. 2007;177:2058–2066. https://doi.org/10.1016/j.juro.2007.01.131
5. Bracke A, Peeters K, Punjabi U, Hoogewijs D, Dewilde S. A search for molecular mechanisms underlying male idiopathic infertility. Reprod Biomed Online. 2018;36:327–339. https://doi.org/10.1016/j.rbmo.2017.12.005
6. Nieschlag E., Behre H.M., Nieschlag S. Andrology. Male Reproductive Health and Dysfunction. Springer Nature Switzerland AG; 2010. https://doi.org/10.1007/978-3-540-78355-8
7. WHO. Infertility: A tabulation of available data on prevalence of primary and secondary infertility. 1991:73. WHO/ MCH/91.9
8. Juul S, Karmaus W, Olsen J. Regional differences in waiting time to pregnancy: pregnancy-based surveys from Denmark, France, Germany, Italy and Sweden. The European Infertility and Subfecundity Study Group. Human Reproduction. 1999;14(5):1250–1254. https://doi.org/10.1093/humrep/14.5.1250
9. Bruckert E. How frequent is unintentional childlessness in Germany? Andrologia. 1991;23:245–250. https://doi.org/10.1111/j.1439-0272.1991.tb02550.x
10. Sabanegh EJ, Agarwal A. Male Infertility in Campbell-Walsh Urology. 10th ed. 2012.
11. WHO laboratory manual for the examination and processing of human semen ‒ 5th ed. 2010. Доступно по: http://apps.who.int/iris/bitstream/10665/44261/1/9789241547789_eng.pdf?ua=1 Ссылка активна на 25.11.2019
12. Bonde JP, Ernst E, Jensen TK, Hjollund NH, Kolstad H, Henriksen TB, Scheike T, Giwercman A, Olsen J, Skakkebaek NE. Relation between semen quality and fertility: A population- based study of 430 first-pregnancy planners. Lancet. 1998;352 (9135):1172–1177. https://doi.org/10.1016/S0140-6736(97)10514-1
13. Guzick DS, Overstreet JW, Factor-Litvak P, Brazil CK, Nakajima ST, Coutifaris C, Carson SA, Cisneros P, Steinkampf MP, Hill JA, Xu D, Vogel DL; National Cooperative Reproductive Medicine Network. Sperm Morphology, Motility, and Concentration in Fertile and Infertile Men. New England Journal of Medicine. 2001;345(19):1388–1393. https://doi.org/10.1056/NEJMoa003005
14. Slama R. Time to pregnancy and semen parameters: a cross-sectional study among fertile couples from four European cities. Human Reproduction. 2002;17:503–515. https://doi.org/10.1093/humrep/17.2.503
15. MacLeod J, Heim LM. Characteristics and variations in semen specimens in 100 normal young men. Obstetrical and Gynecological Survey. 1946;1:447–448. https://doi.org/10.1097/00006254-194606000-00113
16. Carlsen E, Giwercman A, Keiding N, Skakkebaek NE. Evidence for decreasing quality of semen during past 50 years. British Medical Journal. 1992;305:609–613. https://doi.org/10.1136/bmj.305.6854.609
17. Swan SH, Elkin EF, Fenster L. Have sperm densities declined? A reanalysis of global trend data. Environmental Health Perspectives. 1997;105(11):1228–1232. https://doi.org/10.1289/ehp.971051228
18. Swan SH, Elkin EP, Fenster L. The question of declining sperm density revisited: An analysis of 101 studies published 1934‒1996. Environmental Health Perspectives. 2000;108:961–966. https://doi.org/10.1289/ehp.00108961
19. Jorgensen N, Asklund C, Carlsen E, Skakkebaek NE. Coordinated European investigations of semen quality: results from studies of Scandinavian young men is a matter of concern. International Journal of Andrology. 2006;29:54–61. https://doi.org/10.1111/j.1365-2605.2005.00635.x
20. Iwamoto T, Nozawa S, Mieno MN, Yamakawa K, Baba K, Yoshiike M, Namiki M, Koh E, Kanaya J, Okuyama A, Matsumiya K, Tsujimura A, Kanetake H, Eguchi J, Skakkebaek NE, Vierula M, Toppari J, Jørgensen N. Semen quality of 1559 young men from four cities in Japan: a cross-sectional popu lation-based study. BMJ Open. 2013;3(4):e002222. https://doi.org/10.1136/bmjopen-2012-002222
21. Hart RJ, Doherty DA, McLachlan RI, Walls ML, Keelan JA, Dickinson JE, Skakkebaek NE, Norman RJ, Handelsman DJ. Testicular function in a birth cohort of young men. Human Reproduction. 2015;30(12):2713–2724. https://doi.org/10.1093/humrep/dev244
22. Fernandez MF, Duran I, Olea N, Avivar C, Vierula M, Toppari J, Skakkebaek NE, Jørgensen N. Semen quality and reproductive hormone levels in men from Southern Spain. Int J Androl. 2012;35(1):1‒10. https://doi.org/10.1111/j.1365-2605.2010.01131.x
23. Mínguez-Alarcón L, Sergeyev O, Burns JS, Williams PL, Lee MM, Korrick SA, Smigulina L, Revich B, Hauser R. A Longitudinal Study of Peripubertal Serum Organochlorine Concentrations and Semen Parameters in Young Men: The Russian Children’s Study. Environ Health Perspect. 2017;125(3):460‒466. https://doi.org/10.1289/EHP25
24. Takihara H, Cosentino MJ, Sakatoku J, Cockett ATK. Significance of testicular size measurement in andrology: II. Correlation of testicular size with testicular function. Journal of Urology. 1987;137:416–419. https://doi.org/10.1016/S0022-5347(17)44053-5
25. Bahk JY, Jung JH, Jin LM, Min SK. Cut-off Value of Testes Volume in Young Adults and Correlation Among Testes Volume, Body Mass Index, Hormonal Level, and Seminal Profiles. Urology. 2010;75:1318–1323. https://doi.org/10.1016/j.urology.2009.12.007
26. Ruiz-Olvera SF, Rajmil O, Sanchez-Curbelo J-R, Vinay J, Rodriguez- Espinosa J, Ruiz-Castañé E. Association of serum testosterone levels and testicular volume in adult patients. Andrologia. 2018;50:e12933. https://doi.org/10.1111/and.12933
27. Petersen C, Söder O. The Sertoli cell ‒ A hormonal target and “super” nurse for germ cells that determines testicular size. Hormone Research. 2006;66:153–161. https://doi.org/10.1159/000094142
28. Sakamoto H, Yajima T, Nagata M, Okumura T, Suzuki K, Ogawa Y. Relationship between testicular size by ultrasonography and testicular function: Measurement of testicular length, width, and depth in patients with infertility. International Journal of Urology. 2008;15:529–533. https://doi.org/10.1111/j.1442-2042.2008.02071.x
29. Steeno OP. Clinical and Physical Evaluation of the Infertile Male: Testicular Measurement or Orchidometry/Klinische und physikalische Bewertung des infertilen Mannes: Hodenmessung oder Orchidometrie. Andrologia. 1989;21:103–112. https://doi.org/10.1111/j.1439-0272.1989.tb02376.x
30. Schirren C. Exakte Messung der Hodengröße. Andrologia. 1972;4:261–262. (In Germ.).
31. Schonfeld WA, Beebe GW. Normal Growth and Variation in the Male Genitalia from Birth to Maturity. Journal of Urology. 1942;48:759–777. https://doi.org/10.1016/S0022-5347(17)70767-7
32. Lambert B. The frequency of mumps and of mumps orchitis: Consequences for sexuality and fertility. Human Heredity. 1951;2:1–6. https://doi.org/10.1159/000150685
33. Hansen PF, With TK. Clinical Measurements of the Testes in Boys and Men. Acta Medica Scandinavica. 1952;142:457–466. https://doi.org/10.1111/j.0954-6820.1952.tb13395.x
34. Chang KS, Hsu FK, Chan ST, Chan YB. Scrotal asymmetry and handedness. Journal of Anatomy. 1960;94:543–548. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1244352/pdf/janat00442-0104.pdf Accessed November 25, 2019
35. Rundle AT, Sylvester PE. Measurement of testicular volume: Its application to assessment of maturation, and its use in dilation agnosis of hypogonadism. Archives of Disease in Childhood. 1962;37:514–517. https://doi.org/10.1136/adc.37.195.514
36. Farkas LG. Basic morphological data of external genitals in 177 healthy central European men. American Journal of Physical Anthropology. 1971;34:325–328. https://doi.org/10.1002/ajpa.1330340303
37. Johnson L, Petty CS, Neaves WB. Influence of age on sperm production and testicular weights in men. Journal of Reproduction and Fertility. 1984;70:211–218. https://doi.org/10.1530/jrf.0.0700211
38. Wang C, Chan SY, Leung A, Ng RP, Ng M, Tang LC, Ma HK, Tsoi WL, Kwan M. Cross‐sectional study of semen parameters in a large group of normal Chinese men. International Journal of Andrology. 1985;8(4):257–274. https://doi.org/10.1111/j.1365-2605.1985.tb00840.x
39. Handelsman DJ, Staraj S. Testicular Size: The Effects of Aging, Malnutrition, and Illness. Journal of Andrology. 1985;6:144–151. https://doi.org/10.1002/j.1939-4640.1985.tb00830.x
40. Ajmani ML, Jain SP, Saxena S. K. Anthropometric study of male external genitalia of 320 healthy Nigerian adults. Anthropologischer Anzeiger. 1985;43:179–186. Доступно по: https://www.jstor.org/stable/29539617 Accessed November 25.11.2019
41. Centola GM, Lee K, Cockett ATK. Relationship between testicular volume and presence of varicocele. A comparative study. Urology. 1987;30:479–481. https://doi.org/10.1016/0090-4295(87)90386-4
42. Giwercman A, Muller J, Skakkebaek NE. Prevalence of carcinoma in situ and other histopathological abnormalities in testes from 399 men who died suddenly and unexpectedly. Journal of Urology. 1991;145:77–80. https://doi.org/10.1016/S0022-5347(17)38252-6
43. Jit I, Sanjeev. Weight of the testes in Northwest Indian adults. American Journal of Human Biology. 1991;3:671–676. https://doi.org/10.1002/ajhb.1310030618
44. Lenz S, Giwercman A, Elsborg A, Cohr KH, Jelnes JE, Carlsen E, Skakkebaek NE. Ultrasonic testicular texture and size in 444 men from the general population: Correlation to semen quality. European Urology. 1993;24(2):231–238. https://doi.org/10.1159/000474300
45. Spyropoulos E, Borousas D, Mavrikos S, Dellis A, Bourounis M, Athanasiadis S. Size of external genital organs and somatometric parameters among physically normal men younger than 40 years old. Urology. 2002;60:485–489. https://doi.org/10.1016/S0090-4295(02)01869-1
46. Tomova A, Deepinder F, Robeva R, Lalabonova H, Kumanov P, Agarwal A. Growth and Development of Male External Genitalia. Archives of Pediatrics & Adolescent Medicine. 2010;164:1152–1157. https://doi.org/10.1001/archpediatrics.2010.223
47. Aslan Y, Atan A, Ömur Aydn A, Nalçacoǧlu V, Tuncel A, Kadoǧlu A. Penile length and somatometric parameters: A study in healthy young Turkish men. Asian Journal of Andrology. 2011;13:339–341. https://doi.org/10.1038/aja.2010.109
48. Pilatz A, Rusz A, Wagenlehner F, Weidner W, Altinkilic B. Reference values for testicular volume, epididymal head size and peak systolic velocity of the testicular artery in adult males measured by ultrasonography. Ultraschall in Der Medizin. 2013;34:349–354. https://doi.org/10.1055/s-0032-1313077
49. Foresta C, Garolla A, Frigo AC, Carraro U, Isidori AM, Lenzi A, Ferlin A. Anthropometric, penile and testis measures in post-pubertal Italian males. Journal of Endocrinological Investigation. 2013;36(5):287–292. https://doi.org/10.3275/8514
50. Condorelli R, Calogero AE, La Vignera S. Relationship between testicular volume and conventional or nonconventional sperm parameters. International Journal of Endocrinology. 2013;2013:2–7. https://doi.org/10.1155/2013/145792
51. Shalaby ME, Almohsen AE-RM, El Shahid AR, Abd Al-Sameaa MT, Mostafa T. Penile length-somatometric parameters relationship in healthy Egyptian men. Andrologia. 2015;47:402–406. https://doi.org/10.1111/and.12275
52. Tikhonov D.A. The analysis of common and bilateral variability of orchidometric parameters in young men. Morphological newsletter. 2016;24(1):84‒90. (In Russ.). Available at: https://elibrary.ru/download/elirary_25793715_85103585.pdf Accessed November 25, 2019
53. Tillinger K-G. Testicular Morphology. Acta Endocrinologica. 1957;24:S15–192. https://doi.org/10.1530/acta.0.024S015
54. Prader A. Testicular size: assessment and clinical importance. Triangle; the Sandoz Journal of Medical Science. 1966;7(6):240–243. PMID:5920758
55. Dörnberger V, Dörnberger G. Vergleichende Volumetrie des menschlichen Hodens unter besonderer Berücksichtigung der Hodensonographie, Praderorchidometer, Schirrenzirkel und Schublehre*). Andrologia. 2009;19:487–496. (In Germ.).
56. Rivkees SA, Hall DA, Boepple PA, Crawford JD. Accuracy and reproducibility of clinical measures of testicular volume. The Journal of Pediatrics. 1987;110:914–917. https://doi.org/10.1016/S0022-3476(87)80412-2
57. Behre HM, Nashan D, Nieschlag E. Objective measurement of testicular volume by ultrasonography: evaluation of the technique and comparison with orchidometer estimates. International Journal of Andrology. 1989;12:395–403. https://doi.org/10.1111/j.1365-2605.1989.tb01328.x
58. Fuse H, Takahara M, Ishii H, Sumiya H, Shimazaki J. Measurement of testicular volume by ultrasonography. International Journal of Andrology. 1990;13:267–272. https://doi.org/10.1111/j.1365-2605.1990.tb01031.x
59. Sakamoto H, Saito K, Oohta M, Inoue K, Ogawa Y, Yoshida H. Testicular Volume Measurement: Comparison of Ultrasonography, Orchidometry, and Water Displacement. Urology. 2007;69:152–157. https://doi.org/10.1016/j.urology.2006.09.012
60. Rastrelli G, Corona G, Lotti F, Boddi V, Mannucci E, Maggi M. Relationship of Testis Size and LH Levels with Incidence of Major Adverse Cardiovascular Events in Older Men with Sexual Dysfunction. The Journal of Sexual Medicine. 2013;10:2761–2773. https://doi.org/10.1111/jsm.12270
61. Sotos JF, Tokar NJ. Appraisal of testicular volumes: volumes matching ultrasound values referenced to stages of genital development. International Journal of Pediatric Endocrinology. 2017;2017:10. https://doi.org/10.1186/s13633-017-0050-1
62. Oehme NHB, Roelants M, Bruserud IS, Eide GE, Bjerknes R, Rosendahl K, Júlíusson PB. Ultrasound-based measurements of testicular volume in 6- to 16-year-old boys ‒ intraand interobserver agreement and comparison with Prader orchidometry. Pediatric Radiology. 2018;48(12):1771–1778. https://doi.org/10.1007/s00247-018-4195-8
63. Barr ML, Shaver EL, Carr DH, Plunkett ER. the Chromatin‐ Positive Klinefelter Syndrome Among Patients in Mental Deficiency Hospitals. Journal of Intellectual Disability Research. 1960;4:89–107. https://doi.org/10.1111/j.1365-2788.1960.tb00757.x
64. Chaurasia BD, Singh TB. Anthropological data of male external genitals in Central Indian healthy adults. Anthropologischer Anzeiger. 1974;34:210–215. Available at: http://www.jstor.org/stable/29538686 Accessed November 25, 2019
65. Waaler PE, Thorsen T, Stea KF, Aarskog D. Studies in Normal Male Puberty. Acta Paediatrica. 1974;63:1–36. https://doi.org/10.1111/j.1651-2227.1974.tb07587.x
66. Daniel WA, Feinstein RA, Howhrd-peebles P, Ph D, Baxley WD. Clinical and laboratory observations Testicular volumes of adolescents. 1982:0–2. https://doi.org/10.1016/S0022-3476(82)80034-6
67. Skorodok L.M., Savchenko O.N. Disorders of sexual development in boys. [Narushenija polovogo razvitija u mal’chikov]. Moskva: Medicina; 1984. (In Russ.).
68. Taskinen S, Taavitsainen M, Wikström S. Measurement of testicular volume: Comparison of 3 different methods. Journal of Urology. 1996;155:930–933. https://doi.org/10.1016/S0022-5347(01)66349-3
69. Chipkevitch E, Nishimura RT, Tu DGS, Galea-Rojas M. Clinical measurement of testicular volume in adolescents: Comparison of the reliability of 5 methods. Journal of Urology. 1996;156:2050–2053. https://doi.org/10.1016/S0022-5347(01)65433-8
70. Burgart V.Yu., Medvedeva N.N., Zaliznyak I.A. Morphofunctional changing of testicles of Krasnoyars city youths who belong to the different somatotypes. Siberian Medical Review. 2006;39(2):50–52. (In Russ.). Available at: https://elibrary.ru/download/elibrary_15612332_96913888.pdf Accessed November 25, 2019
71. Takihara H, Sakatoku J, Fujii M, Nasu T, Cosentino MJ, Cockett AT. Significance of testicular size measurement in andrology. I. A new orchiometer and its clinical application. Fertility and Sterility. 1983;39:836–840. https://doi.org/10.1016/S0015-0282(16)47126-8
72. Freeman S, Bertolotto M, Richenberg J, Belfield J, Dogra V, Huang DY, Lotti F, Markiet K, Nikolic O, Ramanathan S, Ramchandani P, Rocher L, Secil M, Sidhu PS, Skrobisz K, Studniarek M, Tsili A, Tuncay Turgut A, Pavlica P, Derchi LE; members of the ESUR-SPIWG WG. Ultrasound evaluation of varicoceles: guidelines and recommendations of the European Society of Urogenital Radiology Scrotal and Penile Imaging Working Group (ESUR-SPIWG) for detection, classification, and grading. European Radiology. 2020;30(1):11‒25. https://doi.org/10.1007/s00330-019-06280-y
73. Dooren LJ, Van Gelderen HH, Hamming HD. Testisgrootte en pubesbeharing bij jongens van 10±15 jaar. Ned Tijdschr Geneeskd. 1963;107:1519–1522.PMID: 14045673 (На ни- дерландском).
74. Burr IM, Sizonenko PC, Kaplan SL, Grumbach MM. Hormonal changes in puberty I. Correlation of serum luteinizing hormone and follicle stimulating hormone with stages of puberty, testicular size, and bone age in normal boys. Pediatric Research. 1970;4(1):25–35. https://doi.org/10.1203/00006450-197001000-00003
75. Winter JSD, Faiman C. Pituitary-Gonadal Relations in Male Children and Adolescents. Pediatr Res. 1972;6(2):126‒135. https://doi.org/10.1203/00006450-197202000-00006
76. August GP, Grumbach MM, Kaplan SL. Hormonal changes in puberty: III. correlation of plasma testosterone, LH, FSH, testicular size, and bone age with male pubertal development. Journal of Clinical Endocrinology and Metabolism. 1972;34:319–326. https://doi.org/10.1210/jcem-34-2-319
77. Nielsen CT, Skakkebaek NE, Richardson DW, Darling JA, Hunter WM, Jørgensen M, Nielsen A, Ingerslev O, Keiding N, Müller J. Onset of the release of spermatozia (supermarche) in boys in relation to age, testicular growth, pubic hair, and height. Journal of Clinical Endocrinology and Metabolism. 1986;62(3):532–535. https://doi.org/10.1210/jcem-62-3-532
78. Zhukovskij MA, Lebedev NB, Semicheva TV. Disorders of sexual development. [Narushenie polovogo razvitija]. Moskva: Medicina, 1989. (In Russ.).
79. Béres J, Papp G, Pazonyi I, Czeizel E. Testicular volume variations from 0 to 28 years of age. International Urology and Nephrology. 1989;21:159–167. https://doi.org/10.1007/BF02550804
80. Diamond DA, Paltiel HJ, DiCanzio J, Zurakowski D, Bauer SB, Atala A, Ephraim PL, Grant R, Retik AB. Comparative assessment of pediatric testicular volume: Orchidometer versus ultrasound. Journal of Urology. 2000; 164(3 Pt 2):1111–1114. https://doi.org/10.1097/00005392-200009020-00048
81. Cayan S, Akbay E, Bozlu M, Doruk E, Yildiz A, Acar D, Kanik EA, Ulusoy E. Diagnosis of Pediatric Varicoceles by Physical Examination and Ultrasonography and Measurement of the Testicular Volume. Urologia Internationalis. 2002;69(4):293–296. https://doi.org/10.1159/000066125
82. Karaman MI, Kaya C, Caskurlu T, Guney S, Ergenekon E. Measurement of pediatric testicular volume with Prader orchidometer: Comparison of different hands. Pediatric Surgery International. 2005;21:517–520. https://doi.org/10.1007/s00383-005-1470-1
83. Juul A, Teilmann G, Scheike T, Hertel NT, Holm K, Laursen EM, Main KM, Skakkebæk NE. Pubertal development in Danish children: Comparison of recent European and US data. International Journal of Andrology. 2006;29:247–255. https://doi.org/10.1111/j.1365-2605.2005.00556.x
84. Kuijper EA, van Kooten J, Verbeke JI, van Rooijen M, Lambalk CB. Ultrasonographically measured testicular volumes in 0- to 6-year-old boys. Human Reproduction (Oxford, England). 2008;23:792–796. https://doi.org/10.1093/humrep/den021
85. Goede J, Hack WW, Sijstermans K, van der Voort-Doedens LM, Van der Ploeg T, Meij-de Vries A, Delemarre-van de Waal HA. Normative values for testicular volume measured by ultrasonography in a normal population from infancy to adolescence. Hormone Research in Paediatrics. 2011;76(1):56–64. https://doi.org/10.1159/000326057
86. Osemlak P. Size of testes and epididymes in boys up to 17 years of life assessed by ultrasound method and method of external linear measurements. Medycyna Wieku Rozwojowego. 2011;15:39–55. PMID: 21786511. (in Polish.).
87. Kunde M, Kunze C, Surov A, Ruschke K, Spielmann RP. Sonographische Bestimmung der Hodenmaße im Alter von 0 bis 18 Jahren. Urologe. 2015;54:1772–1778. https://doi.org/10.1007/s00120-015-3810-7
88. Lawal S, Idris HW, Ibinaiye P, Hamidu AU, Tabari MA, Usman B, Lawal AT. Normative ultrasonographic values for testicular volumes in Nigerian boys aged 0‒15 years. Sub-Saharan African Journal of Medicine .2016;3(2):71. https://doi.org/10.4103/2384-5147.184353
89. Wang Y-N, Zeng Q, Xiong F, Zeng Y. Male external genitalia growth curves and charts for children and adolescents aged 0 to 17 years in Chongqing, China. Asian Journal of Andrology. 2018;20:567. https://doi.org/10.4103/aja.aja_51_18
90. Vaganée D, Daems F, Aerts W, Dewaide R, van den Keybus T, De Baets K, De Wachter S., De Win G. Testicular asymmetry in healthy adolescent boys. BJU International. 2018;122:654–666. https://doi.org/10.1111/bju.14174
91. Glazkova A.Je., Danilova L.I., Dudik N.M., Romanovskij A.A. Perculiarities of sexual development and attainment of puberty among Belorussian boys. [Osobennosti polovogo razvitija i stanovlenija pubertata u belorusskih mal’chikov]. Recipe. 2008;60:55–63. (In Russ.). Available at: https://elibrary.ru/download/elibrary_19687690_12518288.pdf Accessed November 25, 2019
92. Stearns EL, MacDonnell JA, Kaufman BJ, Padua R, Lucman TS, Winter JSD, Faiman C. Declining testicular function with age. The American Journal of Medicine. 1974;57:761–766. https://doi.org/10.1016/0002-9343(74)90850-x
93. Baker HWG, Burger HG, de Kretser DM, Hudson B, O’Connor S, Wang C, Mirovics A., Court J., Dunlop M., Rennie G.C. Changes in the Pituitary‐Testicular System With Age. Clinical Endocrinology. 1976;5(4):349–372. https://doi.org/10.1111/j.1365-2265.1976.tb01964.x
94. Handelsman DJ, Staraj S. Testicular Size: The Effects of Aging, Malnutrition, and Illness. Journal of Andrology. 1985;6:144–151. https://doi.org/10.1002/j.1939-4640.1985.tb00830.x
95. Alekseev Y.D., Savenkova E.N., Efimov A.A., Raykova K.A. Comparative analysis of indicators organometrical male gonads person at different ages. Bulletin of Medical Internet Conferences. 2015;5:993–996.(In Russ.). Available at: https://elibrary.ru/download/elibrary_23714602_75725381.pdf Accessed November 25, 2019
96. Aribarg A, Kenkeerati W, Vorapaiboonsak V, Leepipatpaiboon S, Farley TMM. Testicular volume, semen profile and serum hormone levels in fertile Thai males. International Journal of Andrology. 1986;9:170–180. https://doi.org/10.1111/j.1365-2605.1986.tb00880.x
97. Sobowale OB, Akiwumi O. Testicular volume and seminal fluid profile in fertile and infertile males in Ilorin, Nigeria. International Journal of Gynecology and Obstetrics. 1989;28:155–161. https://doi.org/10.1016/0020-7292(89)90476-1
98. Schiff JD, Li PS, Goldstein M. A study from New York was aimed Correlation of ultrasonographic and orchidometer measurements of testis. BJU Int. 2004;93(7):1015‒1057. https://doi.org/10.1111/j.1464-410X.2004.04772.x
99. Cocuzza M, Athayde KS, Agarwal A, Pagani R, Sikka SC, Lucon AM, Srougi M, Hallak J. Impact of clinical varicocele and testis size on seminal reactive oxygen species levels in a fertile population: a prospective controlled study. Fertility and Sterility. 2008;90(4):1103–1108. https://doi.org/10.1016/j.fertnstert.2007.07.1377
100. Iwamoto T, Nozawa S, Yoshiike M, Namiki M, Koh E, Kanaya J, Okuyama A, Matsumiya K, Tsujimura A, Komatsu K, Tsukamoto T, Itoh N, Mieno MN, Vierula M, Toppari J, Skakkebæk NE, Jørgensen N. Semen quality of fertile Japanese men: A cross-sectional population-based study of 792 men. BMJ Open. 2013;3(1). pii: e002223. https://doi.org/10.1136/bmjopen-2012-002223
101. World Health Organization. The influence of varicocele on parameters of fertility in a large group of men presenting to infertility clinics ** Supported by the Special Programme of Research, Development, and Research Training in Human Reproduction, World Health Organization, Geneva. Fertility and Sterility. 1992;57(6):1289–1293. https://doi.org/10.1016/S0015-0282(16)55089-4
102. Costabile RA, Skoog S, Radowich M. Testicular volume assessment in the adolescent with a varicocele. Journal of Urology. 1992;147:1348–1350. https://doi.org/10.1016/S0022-5347(17)37561-4
103. Sadov S, Koskenniemi JJ, Virtanen HE, Perheentupa A, Petersen JH, Skakkebaek NE, Main KM, Toppari J. Testicular growth during puberty in boys with and without a history of congenital cryptorchidism. Journal of Clinical Endocrinology and Metabolism. 2016;101(6):2570–2577. https://doi.org/10.1210/jc.2015-3329
104. Short R V. Testis Size, Ovulation Rate, and Breast Cancer. One Medicine, Berlin, Heidelberg: Springer Berlin Heidelberg; 1984: 32–44. https://doi.org/10.1007/978-3-642-61749-2_4
105. Kabay S, Yucel M, Ozden H, Yaylak F, Ozbek O, Gumusalan Y. Magnetic Resonance Imaging Is a Complementary Method to Stereological Measurement of Testicular Volume. Urology. 2009;73:1131–1135. https://doi.org/10.1016/j.urology.2008.02.058
106. Hsieh ML, Huang ST, Huang HC, Chen Y, Hsu YC. The reliability of ultrasonographic measurements for testicular volume assessment: Comparison of three common formulas with true testicular volume. Asian Journal of Andrology. 2009;11:261–265. https://doi.org/10.1038/aja.2008.48
About the Authors
A. Yu. SeroukhovGhana
Alexander Yurevich Seroukhov ‒ M.D., Specialist Urologist
tel.: +233 50 396 23 35
A. A. Afoko
Ghana
Akisibadek Alekz Afoko ‒ M.D., Cand. Sc.(M); Consultant Urologist, Senior Lecturer
I. E. Mamaev
Russian Federation
Ibrahim Enverovich Mamaev ‒ Head, Urology Division; M.D., Cand. Sc. (M), Ass. Prof.; Ass. Prof., Dept. of Urology and Andrology
Review
For citations:
Seroukhov A.Yu., Afoko A.A., Mamaev I.E. Global Secular Trend of Gonadal Size in Men: Review and Analysis of Publications. Urology Herald. 2020;8(1):75-91. https://doi.org/10.21886/2308-6424-2029-8-1-75-91













































