Scroll to:
Buccal dorsal augmentation ureteroplasty for extended ureteral stricture having an obliteration site
https://doi.org/10.21886/2308-6424-2025-13-1-77-81
Abstract
Buccal ureteroplasty is a surgery that is now increasingly encountered in urological practice. There are various techniques for performing this surgical procedure, which require further improvement. This article presents a clinical case and the immediate results of ureteroplasty utilising the oral mucosa via the augmentation anastomosis technique in a 40-year-old patient with an extended recurrent ureteral stricture having an obliteration site.
For citations:
Volkov A.A., Mustapaev I.D., Mirzaev Z.A., Muziev A.V. Buccal dorsal augmentation ureteroplasty for extended ureteral stricture having an obliteration site. Urology Herald. 2025;13(1):77-81. https://doi.org/10.21886/2308-6424-2025-13-1-77-81
Introduction
In recent decades many urologic invasions are made without traditional surgery sections, but with the help of laparoscopic and robotic techniques, and the achievements in laparoscopic urology show wide opportunities for ureteral reconstructive surgery with respective results in comparison with similar open surgery [1].
Using of oral cavity’s graft — buccal grafting (BG) — in surgical treatment of extended strictures and ureteral obliterations is not a rare case in reconstructive surgery anymore. Substitution of ureter’s defect with BG can be implemented in any of its departments, and this operation is used as a variant of ureter’s reconstruction under the high risks in intestinal ureteral plastics and kidney transplant surgery [2]. The main techniques of buccal ureteroplasty are onlay — partial replacement of upper urinary tract tissue and tubularisation — as complete tissue replacement to form a tubular graft [3]. In some cases, if obliteration part is short, the dissection of the affected area together with making ureter’s terminal anastomosis on the one side and BG substitution of ureter’s trance defect on the other side is possible [4][5]. This method is known as augmentation anastomosis due to its analogy with surgical technique used on ureteral strictures [6].
Objective. To present a clinical case of a patient with an extended recurrent ureteral stricture having an obliteration site, who underwent buccal ureteroplasty using the augmentation anastomosis technique in its own modification.
Patient’s information
A 40-year-old man presented with complaints about the presence of a nephrostomy placed for left-sided acute obstructive pyelonephritis. For 10 years patient suffers long-term urolithiasis. The discharge of left kidney’s stones and pyelonephritis attacks were repeatedly noticed. In July 2014 the patient has undergone ureterolithotripsy, stenting of left ureter. Renal colic repeated in January 2023. During the examination the middle third of the left ureter’s stone has been detected. Surgical intervention, namely, laser ureterolithotripsy on the left has been implemented. In September 2023 the patient has developed acute obstructive pyelonephritis on the left, percutaneous puncture nephrostomy has been made. During further examination the diagnosis of long-term stricture of the mid-third of the left ureter with obliteration site (Fig. 1).
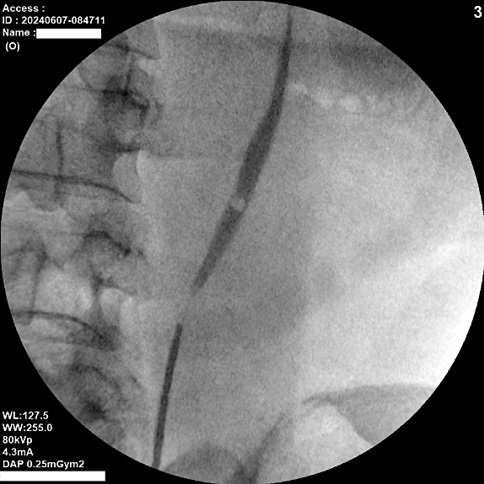
Figure 1. Retrograde ureterogram + antegrade pyeloureterogram of ureteral stricture with an obliteration site before surgery
Рисунок 1. Ретроградная уретерограмма + антеградная пиелоуретерограмма стриктуры мочеточника с участком облитерации до оперативного вмешательства
Сlinical case
The patient arrived in Surgery Center of the “Military Veterans Hospital” in Rostov region. Reconstruction of the middle third of ureter has been performed. The affected ureter was previously catheterized, the end catheter was conducted to the obliteration site. Gas insufflated into the abdominal cavity, and 4 ports were placed in the abdomen. The affected area of the middle third of the left ureter was detected intraperitoneally, scar-altered fiber was removed from its surface and, the ureter was crossed in the projection of obliteration focusing on the end catheter. The scar tissue is excised from the ends of ureter up to the appearance of its lumen. Dissected ureter’s distal and proximal edges were spatulated to 10 mm along the posterolateral surface. Then the ureter was excreted in distal and proximal directions within healthy tissue up to reaching free connection of anteromedial edges of the resected ureter. Diamond-shaped mucosal autograft sampling in oral cavity has been carried out. Autograft length was determined by the length of ureteral defect, calculated during the connection of anteromedial edges of distal and proximal ureteral ends, maximum autograft width reached 20 mm. Buccal autograft was cleared from muscle tissue. A monocryl suture 4-0 («Ethicon Inc.», Johnson & Johnson Company, Cincinnati, OH, USA) was applied on the free edge, the autograft was immersed in the abdominal cavity via laparoscopic port. Using monocryl 4-0 BG was fixed to ureteral distal edge with single suture on its posterior surface to the angle of the incision, made during spatulation with lumbar muscle capture.
The BG was fixed using single sutures (Monocryl 4/0) to the surface of the lumbar muscle with the epithelium directed into the ureteral lumen, leaving its edges free. Internal drainage stent was implanted through the ureteral distal lumen along the proximal ureteral edge to pelvis, anastomosis of ureter’s ends was made on anteromedial surface by two singular monocryl 4/0 sutures, buccal autograft and dissected ureteral parts were sutured over the stent by continuous external monocryl 4/0 suture (Fig. 2). The drainage was installed into the abdominal cavity.
The early postoperative period was favourable. Drainage was removed on the 3-day due to the minimum discharge. Ureteral stent was removed after six weeks. During the control ultrasound of kidneys in 1, 3, 6 weeks after stent removal no increase in hydronephrosis on the left was deduced. Left retrograde ureteropyelography was performed at six months of follow-up (Fig. 3), under which the patency of the anastomosis area is determined.
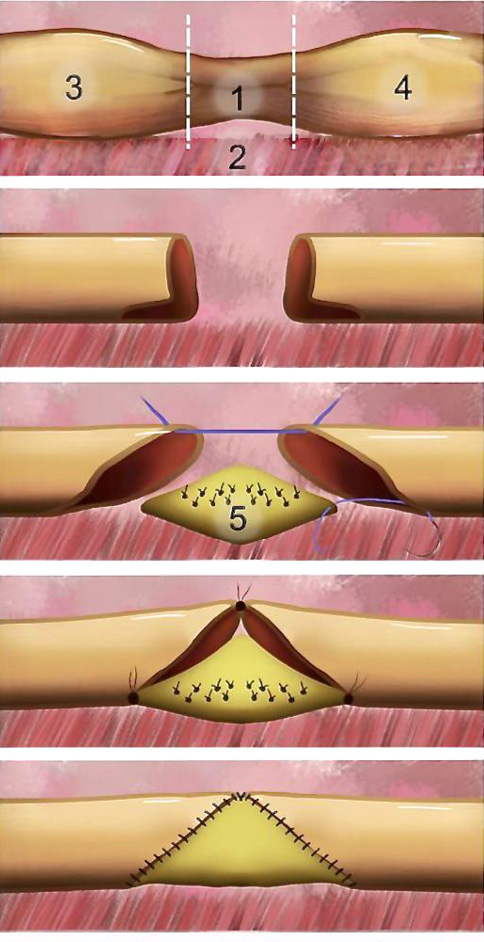
1 — Cтриктура с облитерацией; 2 — Поясничная мышца; 3, 4 — Дистальный и проксимальный концы мочеточника; 5 — Графт
Figure 2. Stages of ureteral reconstruction using a buccal graft: A — ureteral stricture with obliteration; B — ureteral obliteration area excised, ureteral spatulation performed; C — fixation of buccal graft to lumbar muscle; D — upper ureteral semicircle sutured using knotted sutures following subsequent graft fixation; E — final view of ureteral reconstruction
Рисунок 2. Этапы реконструкции мочеточника с использованием буккального графта:
A — участок стриктуры мочеточника с облитерацией; B — участок облитерации мочеточника иссечён, выполнена спатуляция мочеточника; C — фиксация буккального графта к поясничной мышце; D — верхняя полуокружность мочеточника ушита узловыми швами с последующей фиксацией графта; E — окончательный вид реконструкции мочеточника

Figure 3. Retrograde ureterogram showing the reconstruction site six months after surgery
Рисунок 3. Ретроградная уретерограмма участка реконструкции через шесть месяцев после оперативного вмешательства
Discussion
Y. You et al. (2023) carried out the analysis to compare the results of buccal urethroplasty and urethroplasty using the segment of the ileum. It is shown that buccal urethroplasty in all its variants is the effective, minimally invasive and having relatively low percent of complications operation, which is safer than the reconstruction of ureter by using intestinal segments. This operation, according to the authors’ idea, is the preferable treatment method of extended ureteral strictures up to 80 mm [7].
However buccal urethroplasty on the method of augmentative anastomosis is the least studied variant of such an operation. Present technique of augmentative anastomosis in ureteroplasty with using BG includes following stages: using the open access, excision of pathologically altered area of the ureter, creating an anastomosis on the posterior ureter’s surface, replacement of the defect of the anterior ureteral surface with oral mucosa and wrapping an omentum tissue around the surgery site [8][9]. At the same time, the drawbacks of this technique, in our opinion, are weak degree of autotransplant vascularization by omentum tissue and excessive injury during the operation made by open access. It is well-known, that for BG muscular tissue is a better variant in terms of neoangiogenesis, that the adipose one [10]. Augmentative anastomosis can be a reasonable alternative to tabular BG in ureteroplasty, as most authors consider, that tabularization of autograft with oral mucosa further leads to increased recurrence of upper urinary tract obstruction [11][12].
In our clinical cases study, we presented buccal ureteroplasty using the technique of augmentation anastomosis with dorsal location of the BG. This operation was performed using techniques aimed at improving the patient's quality of life and preventing possible postoperative complications and recurrence of upper urinary tract obstruction - laparoscopic access, minimal tissue dissection with removal of only the obliterated area, additional vascularisation of the BG with muscle tissue. Anastomosis of ureteral ends in this case is applied along the anterior surface of the ureter and the length of the BG is determined by the possibility of juxtaposition of the ureteral ends without tension.
Conclusion
The presented buccal ureteroplasty technique will contribute to further refinement of this operation to reduce invasiveness and improve outcomes. Ongoing studies will help to define the role of this technique in patients with prolonged upper urinary tract obstruction.
References
1. Gild P, Kluth LA, Vetterlein MW, Engel O, Chun FKH, Fisch M. Adult iatrogenic ureteral injury and stricture-incidence and treatment strategies. Asian J Urol. 2018;5(2):101-106. DOI: 10.1016/j.ajur.2018.02.003
2. Volkov A.A., Budnik N.V., Zuban O.N. Optimization of laparoscopic ureteral repair with a buccal graft in case of its extended strictures and obliterations. Research and Practical Medicine Journal. 2021;8(3):52-61. (In Russian). DOI: 10.17709/2410-1893-2021-8-3-5
3. Volkov A.A., Budnik N.V., Zuban O.N., Mustapaev I.D., Abdulaev M.A., Muziev A.V. Buccal ureteroplasty options, techniques, long-term results. Research and Practical Medicine Journal. 2022;9(2):86-95. (In Russian). DOI: 10.17709/2410-1893-2022-9-2-7
4. Naude JH. Buccal mucosal grafts in the treatment of ureteric lesions. BJU Int. 1999;83(7):751-754. DOI: 10.1046/j.1464-410x.1999.00019.x
5. Katibov M.I., Bogdanov A.B., Dovlatov Z.A. Ureteroplasty using oral mucosa graft: a literature review. Update in 2022. Urology Herald. 2022;10(3):84-97. (In Russian). DOI: 10.21886/2308-6424-2022-10-3-84-97
6. Redmond EJ, Hoare DT, Rourke KF. Augmented Anastomotic Urethroplasty is Independently Associated with Failure after Reconstruction for Long Bulbar Urethral Strictures. J Urol. 2020;204(5):989-995. DOI: 10.1097/JU.0000000000001177
7. You Y, Gao X, Chai S, Chen J, Wang J, Zhang H, Zhou Y, Yu Z, Cheng G, Li B, Xiao X. Oral mucosal graft ureteroplasty versus ileal ureteric replacement: a meta-analysis. BJU Int. 2023;132(2):122-131. DOI: 10.1111/bju.15994
8. Fan S, Yin L, Yang K, Wang J, Li X, Xiong S, Yu X, Li Z, Guan H, Zhu H, Zhang P, Li X, Zhou L. Posteriorly Augmented Anastomotic Ureteroplasty with Lingual Mucosal Onlay Grafts for Long Proximal Ureteral Strictures: 10 Cases of Experience. J Endourol. 2021;35(2):192-199. DOI: 10.1089/end.2020.0686
9. Reyad AM, Abd Elhamed AM, Elsherief AM, Abdelhaleem HA, Mahmoud TA. Augmented anastomotic ureteral reconstruction using buccal mucosal graft, initial experience. Urologia. 2024;91(3):611-616. DOI: 10.1177/03915603241241829
10. Belomyttsev S.V. Clinical and morphological rationale of using mucosal grafts for urethroplasty in men [dissertation]. Moscow; 2012. (In Russian). URL: http://www.dslib.net/urologia/kliniko-morfologicheskoe-obosnovanie-ispolzovanija-svobodnyh-slizistyh-loskutov.html
11. Gonzalez AN, Mishra K, Zhao LC. Buccal Mucosal Ureteroplasty for the Management of Ureteral Strictures: Patient Selection and Considerations. Res Rep Urol. 2022;14:135-140. DOI: 10.2147/RRU.S291950
12. Xiong S, Wang J, Zhu W, Yang K, Ding G, Li X, Eun DD. Onlay Repair Technique for the Management of Ureteral Strictures: A Comprehensive Review. Biomed Res Int. 2020;2020:6178286. DOI: 10.1155/2020/6178286
About the Authors
A. A. VolkovRussian Federation
Andrey A. Volkov — Dr.Sc.(Med)
Rostov-on-Don
I. D. Mustapaev
Russian Federation
Irbajhan D. Mustapaev
Rostov-on-Don
Z. A. Mirzaev
Russian Federation
Zaur A. Mirzaev — Cand.Sc.(Med)
Rostov-on-Don
A. V. Muziev
Russian Federation
Ahmed V. Muziev
Rostov-on-Don
Review
For citations:
Volkov A.A., Mustapaev I.D., Mirzaev Z.A., Muziev A.V. Buccal dorsal augmentation ureteroplasty for extended ureteral stricture having an obliteration site. Urology Herald. 2025;13(1):77-81. https://doi.org/10.21886/2308-6424-2025-13-1-77-81













































